Why Many Say No to Addiction Treatment
The most common reasons for avoiding treatment for illicit substance use were denial of a problem, concerns about privacy, and fear.

Read Time: 2 minutes
Published:
For the first time in years, drug overdose deaths in the United States are rising again, with 1,400 more fatalities in the last year alone. Yet many who could benefit from treatment never seek it, most often because they do not believe they have a problem. Media influence and peer pressure have normalized drug use in social settings, making it harder to recognize when usage shifts from casual to problematic.
The belief that one does not have addiction remains a major barrier, even as effective medications and interventions exist to support recovery. This perception drives treatment avoidance, compounded by a lack of insurance or access to treatment.
Systemic challenges include treatment cost and location, which further compound mistrust in health care. Culturally competent care—such as programs with bilingual providers or peer support—can help patients from marginalized populations feel acknowledged, making them more likely to engage in care.
A recent study surveyed 858 patients who received interventions for illicit drug use across 6 emergency departments between 2010 and 2012. To understand barriers to entering treatment for the first time, the researchers focused on adult patients who were not actively seeking care and who used substances other than alcohol and tobacco in the past 30 days.
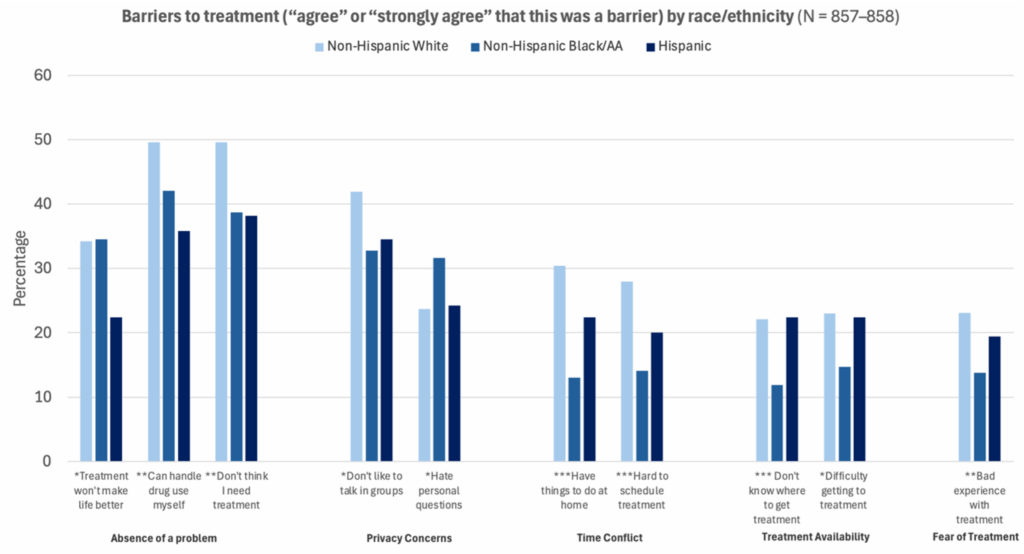
Among the patients, the most common reasons for avoiding treatment were denial, privacy concerns, and fear, as shown in the graph above. These reasons were consistent across all racial and ethnic groups, although some differences appeared. Non-Hispanic White patients more often cited self-reliance; Black patients raised greater privacy concerns (ex., discomfort with personal questions); and Hispanic patients noted time limitations and fear of family disapproval.
While the data are over a decade old, the patterns they reveal remain relevant today. The findings show how treatment barriers are both deeply personal and structurally entrenched. Recent efforts have increased treatment availability and medication prescriptions. But many still struggle to recognize their addiction, indicating how strongly beliefs shape treatment avoidance.
By recognizing denial as a barrier, clinicians can design environments that invite more people into care. Regular screenings can help recognize problematic drug use, and culturally competent counseling can address diverse patients. Building trust, practicing cultural humility, and easing the burden of disclosure can reshape how substance use treatment is offered so people can feel seen and willing to begin.
This is the first piece in a three-part series on substance use disorder and treatment. Read part two and part three.



