Physician Burnout: When Paperwork Undermines Patient Care
Insurance-related paperwork is a key driver of physician burnout, with clear downstream harms on patient care and efficiency.
Read Time: 4 minutes
Published:
Throughout their careers, clinicians are often asked, “Why medicine?” Many express a desire to help people as their primary motivator for entering the field. But over time, this motivation is tested by mounting administrative demands and emotional strain, fueling the rising rates of physician burnout. Between 2011 and 2021, the rate of burnout rose by 17%—a troubling trend with far-reaching implications for patient care and health systems.
Health care environments place physicians at high risk for burnout, which is a long-term occupational stress reaction characterized by emotional, physical, and mental exhaustion. Early signs include emotional exhaustion, where ongoing stress leaves physicians feeling drained, and depersonalization, which can manifest as reduced empathy, emotional detachment, and a diminished sense of accomplishment. As burnout deepens, physicians experience impaired attention, memory, and executive functioning.
Contributing factors include time pressures, limited autonomy, chaotic workplaces, and poor culture. Electronic medical records intensify the strain, requiring clinicians to document efficiently while managing high patient volumes. Staffing shortages lead to shorter appointments and greater chaos, while weak communication and poor team cohesion further reduce physicians’ sense of autonomy. A growing source of burnout is administrative burden, particularly that imposed by insurance-mandated practices.
Physician burnout is not a reflection of individual competence or resilience, but a symptom of broader systemic inefficiencies.
Health insurance companies use specific tactics—known as utilization management—that influence patient care decisions to control overall medical expenditures. These techniques, however, inadvertently shift physicians’ focus from patient care to paperwork. For example, before prescribing a medication, physicians must request the patient’s insurance provider for approval. Since approval hinges on precise documentation and criteria, the process can be burdensome and time-consuming, often requiring repeated appeals.
Similarly, health insurers require physicians to prescribe a sequence of insurer-preferred medications before they will cover the initially recommended medication. Patients must trial and fail a lower-tier drug before accessing a higher-tier one, regardless of medical history or needs. In some cases, insurers require physicians to switch patients from a stable, effective medication to a preferred, lower-cost alternative, often for non-clinical reasons and against medical advice.
To understand the burden of time-consuming administrative tasks, Arwen Struthers and associates surveyed 501 U.S. physicians, primarily in general medicine, on how prior authorization, step therapy, and non-medical switching contribute to burnout. The majority reported all three practices as barriers to patient care and clinic workflow, with 77% citing prior authorization as the greatest barrier. Over half of the respondents spent 6 to 21 hours per week filling out insurance-related paperwork. Nearly three-fifths (58%) hired extra staff to manage these tasks as they were unable to complete them during normal working hours.
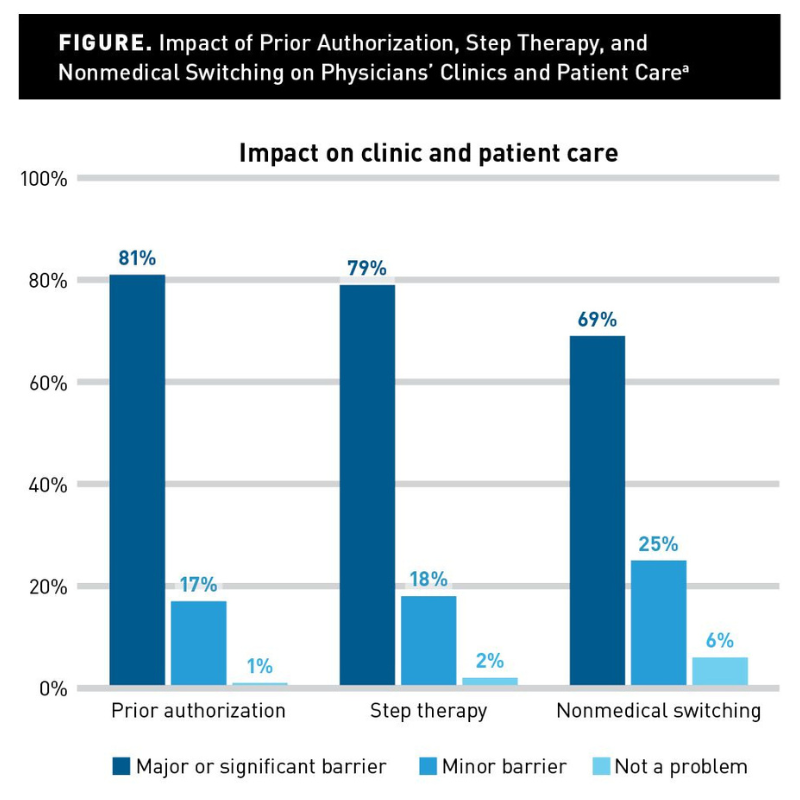
Nearly half of the surveyed physicians (48%) reported currently experiencing burnout, while 37% had experienced it in the past. Those with burnout were more likely to rush patient visits, increasing the risk of missed diagnoses. Notably, 88% of physicians felt they could provide better care if freed from burdensome tasks. The findings point to insurance-related paperwork, particularly prior authorization and step therapy, as a major driver of burnout, with clear downstream harms on care quality and efficiency.
The authors urge health insurance reform as one strategy to restore physician autonomy. Proposed changes include streamlining prior authorization and appeals, prioritizing medical need over cost containment, and exempting previously approved medications from step therapy when patients change insurers.
Policy changes have already begun: starting in 2026, a new Center for Medicare & Medicaid Services rule will require faster prior authorization decisions. The policy mandates insurers to deliver a decision within seven days of a request, which can be further expedited to 72 hours based on urgency. To improve transparency and accountability, insurers must also publicly report approval and denial metrics, including detailed reasons for denial.
Physician burnout is not a reflection of individual competence or resilience, but a symptom of broader systemic inefficiencies. Revisiting strategies to address physician burnout is essential to their professional well-being, as well as for the health of the patients they serve. In doing so, they may reconnect with their original answer to the question “Why medicine?”



