Unjust Deserts
One in three United States counties qualifies as a maternity care desert, defined by a complete absence of obstetric providers and care at hospitals or birthing centers.
Read Time: 2 minutes
Published:
Most pregnancies require upwards of 10 check-ups. Regular prenatal care visits that include education and counseling improve the chances of healthy pregnancy, reducing risk of complications during pregnancy and at birth by monitoring health for all stages of fetal growth. Yet maternal mortality in the United States is climbing.
There were 32.9 deaths per 100,000 live births in 2021, a marked increase from 20.1 per 100,000 in 2019. Black mothers experienced 2.6 times higher death rates than White mothers, at 70 deaths per 100,000 live births. Currently, the U.S. has the highest pregnancy-related death rate of all high-income democracies.
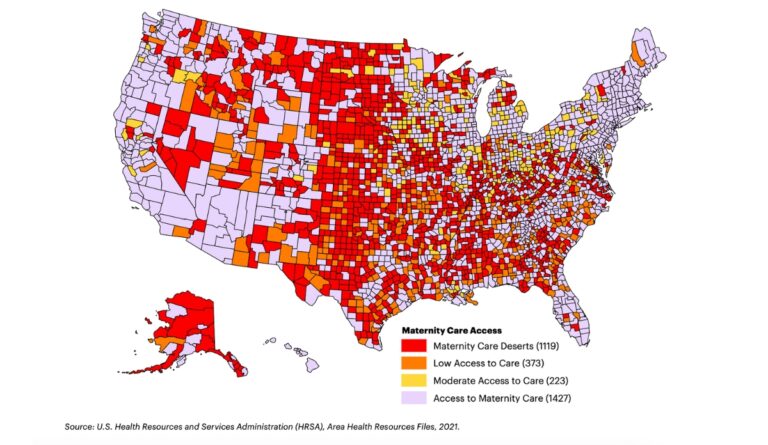
One major barrier preventing access to regular, quality prenatal care is the convenience of patients getting to medical offices. Many counties in the U.S. qualify as maternity care deserts, defined by a complete absence of obstetric providers (e.g. obstetricians, gynecologists, or certified nurse midwives) and obstetric care at hospitals or birthing centers.
The figure above, presented in March of Dimes’ 2022 Maternity Care Report, utilized Area Health Resource Files data from the U.S. Health Resources and Services Administration. The map shows each of the 3,142 U.S. county’s status according to its maternity care access. One in three counties qualifies as a maternity care desert, as shown in red. Notably, areas with more deserts and higher maternal and infant deaths also have restrictive abortion policies.
Policy changes can effectively prevent maternity care deserts, and the Biden administration has begun to take action. Increased availability of diversified obstetric providers (like midwives and doulas for low-risk pregnancies) could reduce the dearth of available personnel. Better insurance by public and private payers could cover births at reasonable costs and expand services to include midwifery. More clinics opening up in remote areas could assist in bolstering federal initiatives like the Rural Maternity and Obstetrics Management (RMOM) Program, which focuses on improving telehealth and coordinated care for patients to reduce maternal mortality.
Maternity care deserts can be transformed into places of care–it all comes down to how effective policy can be delivered to entice providers and clinics to open new doors to regular prenatal care.
Databyte via Christina Brigance, Ripley Lucas, Erin Jones, et al. Nowhere to Go: Maternity Care Deserts Across the U.S. (Report No. 3). March of Dimes, 2022.



