The Silent Pain of IUDs
Over 40% of study participants reported experiencing unacceptable levels of pain related to intrauterine device (IUD) insertion.

Read Time: 3 minutes
Published:
Almost a quarter of reproductive-age women in the United States have an intrauterine device (IUD), a flexible, T-shaped device placed in the uterus to prevent pregnancy. Its long-acting, reversible nature makes it appealing, offering up to 10 years of contraception. But in reality, IUD insertion can be remarkably painful, deterring people from using this highly effective and convenient method.
Historically, IUD pain has been downplayed. The discomfort is dismissed as brief or not clinically severe. Patients are often directed towards over-the-counter medications despite reporting pain that warrants more concern. Firsthand accounts describe severe cramping, bleeding, and even fainting during the procedure.
These experiences are not isolated. Rather, they reflect broader disparities in how pain is treated. For instance, women are less likely than men to receive opioids or numbing agents for chronic pain. Low-income patients also receive far fewer prescriptions than their high-income peers due to insurance constraints or inability to pay out of pocket for anesthesia. Likewise, Black patients are less likely than White patients to be referred to pain specialists, despite undergoing similar procedures.
To further deduce these inequities, Alexandra Garo and associates assessed the experiences of 620 IUD recipients from the HER Salt Lake Contraceptive Initiative from 2016 to 2019. Participants rated their pain and anxiety levels on a linear 100-point scale. They were grouped based on whether they deemed their pain acceptable or unacceptable. They also reported pain management options they had been offered and those they would have preferred.
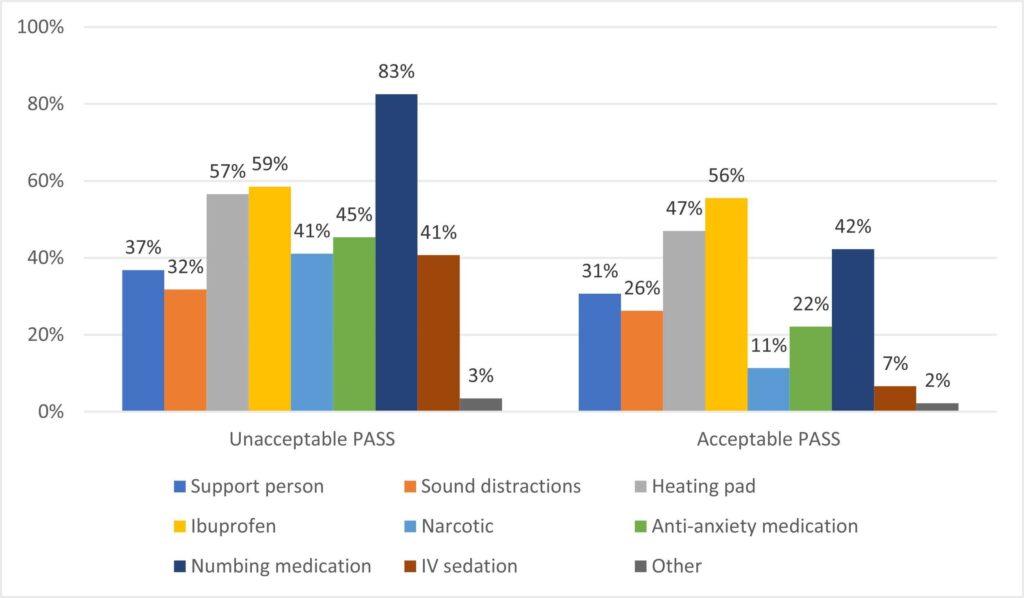
Over 40% of participants experienced unacceptable insertion pain. Their pain scores averaged 27.42 points higher compared to those with acceptable pain. Nearly half (47.7%) reported anxiety, and one-third (33.7%) disclosed a history of trauma, showing how personal experiences shape pain perception. When asked about pain relief options, most participants felt that numbing, ibuprofen, or heating pads would be helpful—but more than half were not offered any options.
The results highlight the need for more patient-centered pain management, particularly for women. Although federal guidelines say private insurers must cover contraceptive care, states can loosely interpret whether this includes pain management. This year, Massachusetts introduced Bill H.1315 to mandate comprehensive coverage of pain management for IUD insertion, effective in 2026. It is currently under review.
The CDC and the American College of Obstetricians and Gynecologists have also updated their IUD recommendations. They encourage clinicians to openly discuss pain expectations and offer evidence-based options, such as topical lidocaine and paracervical blocks. This marks an earnest step forward and offers patients a hopeful sign that their voices are being heard.



