The Hidden Inequity in Emergency C-Sections
Among low-risk pregnant mothers, Black mothers were 149% more likely than White mothers to undergo an unscheduled C-section.

Read Time: 2 minutes
Published:
Cesarean deliveries in American hospitals have risen dramatically, from 20.7% in 1996 to 32.1% in 2021—more than double the 10-15% rate that the World Health Organization considers medically optimal.
When medically necessary, C-sections save lives. However, like any major surgery, they carry risks including longer recovery times and increased dangers in future pregnancies. This makes the timing and necessity of C-sections crucial medical decisions—decisions that appear to be influenced by race.
Adriana Corredor-Waldron and colleagues examined this disparity through nearly one million birth records from New Jersey hospitals between 2008 and 2017. They focused on unscheduled C-sections—surgeries performed after a mother has gone into labor naturally, rather than being planned in advance. These procedures represent real-time medical decisions, making them useful for studying how doctors respond to medical situations during labor.
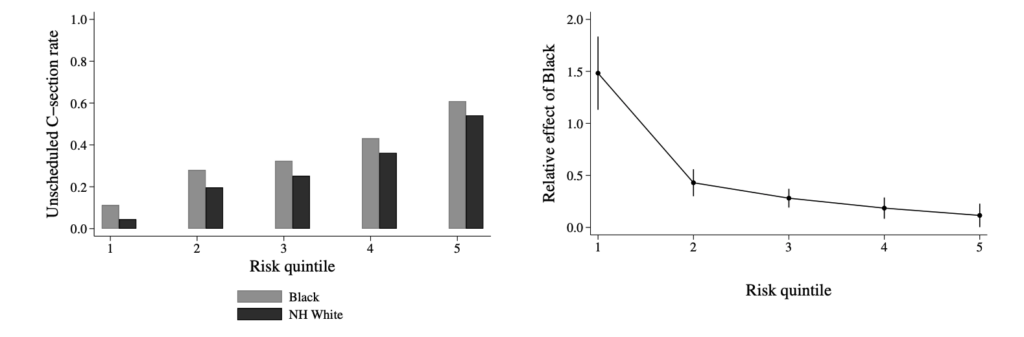
The graphs above illustrates racial disparities across five levels of medical risk. Among mothers with the lowest risk factors, Black mothers were 149% more likely than White mothers to undergo an unscheduled C-section. This gap could not be explained by differences in medical risk factors, insurance coverage, education levels, or choice of hospital or doctor. In fact, Black mothers in the study were generally younger and had fewer risk factors for C-sections.
Most revealing was what happened when hospitals were busy: when operating rooms were occupied with scheduled procedures, the racial disparity in unscheduled C-section rates virtually disappeared—without any increase in complications. This suggests that when resources are constrained, doctors become more selective, performing Cesarean deliveries only when medically necessary.
These findings point to a complex form of racial inequity in medical decision-making. Rather than denying necessary care, providers appear more likely to perform additional, potentially unnecessary surgeries on Black mothers when resources allow. This highlights the urgent need for health care systems to implement more standardized protocols for determining when C-sections are truly necessary.



