More Young Adults Try PrEP, Fewer Stick With It
Only 36% of people who could benefit from PrEP continually use it, and rates are especially low among the youngest adults.

Read Time: 2 minutes
Published:
Decades of progress in HIV prevention and treatment in the United States have yielded dramatic improvements. Annual diagnoses dropped from nearly 80,000 in the 1980s to 31,800 in 2022.
But HIV, which is primarily transmitted through sex or injection drug use, continues to impact thousands of Americans every year. Those at higher risk include people who have unprotected sex, multiple partners, or limited access to sexual health care.
Pre-exposure prophylaxis (PrEP) is a key prevention strategy that has dramatically expanded HIV prevention options in the U.S. Taken once daily or on-demand, PrEP reduces the risk of sexually transmitted HIV infection by 99% and is covered by most insurers. Yet uptake remains low. Only 36% of people who could benefit from PrEP use it, and rates are especially low among sexually active minors and young adults, Black and Latino patients, those with public insurance, and people living in the South.
In a new study, Nina Hill and colleagues looked at national PrEP use trends among young adults ages 18-25. Using data from the IQVIA Longitudinal Prescription Database, the researchers tracked three key measures between 2016 and 2023: how many people filled prescriptions for PrEP (dispensing), how many started it for the first time (initiation), and how long they continued to take it (persistence).
Over the study period, PrEP prescription fills increased roughly 700%, growing quickly from 2016 to 2018, then more gradually. The number of new users followed a similar trend. However, the average amount of time people stayed on PrEP dropped from 112 days in 2016 to 98 days in 2023. The authors hypothesized that patients may discontinue PrEP because they lack follow-up care or are using it on-demand rather than daily.
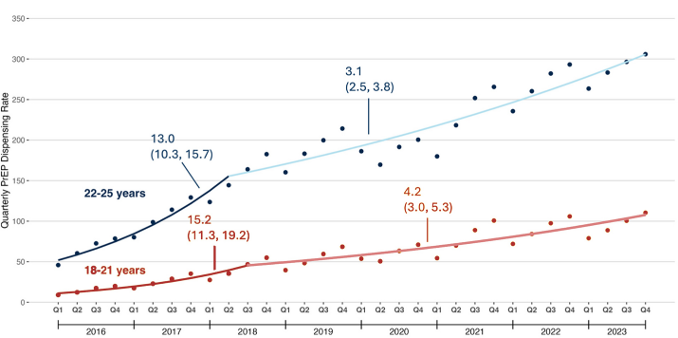
The youngest adults, aged 18 to 21, were less likely to start or continue PrEP compared to those aged 22-25. The authors suggest this could be because younger patients might see pediatricians, who would be less familiar with prescribing PrEP. They may also worry about privacy, especially if they use a parent’s health insurance. Or they might hold misconceptions about PrEP, such as believing it is only for LGBTQIA individuals.
The study highlights the need for targeted interventions to improve PrEP persistence and reduce access barriers. As HIV prevention efforts evolve, ensuring that young adults can start and stay on PrEP remains critical to ending the epidemic.



