The Devastating Toll of Structural Racism
Structural racism is a root cause of adverse Covid-19 outcomes among older Black and Latinx adults.

Read Time: 4 minutes
Published:
A preponderance of evidence indicates structural and economic inequalities in America disproportionately impact the health and wellbeing of Black and Latinx older adults.
Structural racism refers to the way current and historical institutions and public policies can produce outcomes that perpetuate racial/ethnic inequity and normalize the mistreatment and acceptance of worse outcomes for people of color. Before the pandemic, the unjust treatment of Black and Latinx populations included discriminatory governmental policies (Jim Crow and the New Deal), and unfair institutional practices (predatory lending, residential segregation, and access to affordable high-quality healthcare). These historical and ongoing structural forces created a fundamentally unequal health landscape that resulted in an accumulation of health disadvantages among older cohorts of Black and Latinx adults.
Long-standing and deeply rooted racial/ethnic disparities stem from structural racism in a host of societal domains (education, employment, criminal justice, health care systems, and housing). Structural racism contributes to different levels of health risks over time for older Black and Latinx adults compared to older white adults. Due to constrained socioeconomic opportunities, and limited access to healthcare and health-promoting resources, Black and Latinx adults spend a larger proportion of their remaining life after age 50 with debilitating health conditions such as cancer, diabetes, dementia, disability, heart disease, hypertension, and stroke than white adults.
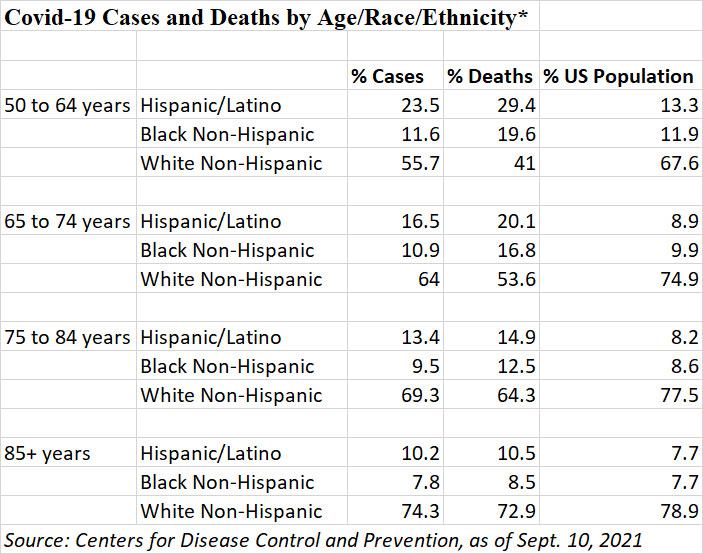
Mounting evidence documents stark racial/ethnic inequalities in the number of confirmed infections, hospitalizations, and deaths from Covid-19.
These findings have highlighted the harsh reality that structural racism is also a root cause of adverse Covid-19 outcomes among older Black and Latinx adults. Recent data indicate that the percentage of Covid-19 cases and deaths among older Black and Latinx adults continues to exceed their percentage of the population.
Similarly, hospitalization rates are approximately 2 times higher for older Black and older Latinx adults than older white adults. Nursing homes with higher proportions of minority residents also experience more Covid-19 infections and deaths than those with high proportions of white residents. Furthermore, Black and Latinx adults report greater access-related barriers to receiving a Covid-19 vaccine than white adults.
The disproportionate effect of Covid-19 on older minorities highlighted above reflects systemic inequalities that place older Black and Latinx adults at greater risk as the highly contagious Delta variant spreads across the US. For example, residential segregation and long-term disinvestment in communities of color may contribute to older Black and Latinx adults’ lower access to testing, vaccination sites, or quality and culturally-appropriate social service providers to assist with scheduling and transportation to testing or vaccination sites.
Looking forward, public health practitioners have a key role to play in addressing the systemic drivers of Covid-19 on older Black and Latinx communities. As the Delta variant drives up infections, hospitalizations, and deaths, many older adults remain unvaccinated and highly vulnerable.
Public health approaches to outreach, education, and vaccine administration should prioritize the needs of communities of color, including older Black and Latinx adults who remain highly susceptible to negative Covid-19 outcomes, particularly with the rollout of booster shots for fully vaccinated individuals in the coming months. This may include ensuring that vaccination sites are located conveniently for older Black and Latinx adults and that sign-up processes are accessible, streamlined, and offer support for scheduling appointments and transportation if available. Vaccine outreach should be conducted in partnership with trusted community leaders. And public health efforts to address vaccine hesitancy should acknowledge the historical and ongoing medical mistreatment of people of color that contributes to mistrust of medical institutions..
Meaningful progress towards health equity will require systemic changes beyond the scope of pandemic response measures or traditional public health policy. Structural policy changes to reduce racial/ethnic inequality are urgently needed, including universal healthcare coverage, robust investment in affordable housing and social services in communities of color, and poverty-reducing policies such as baby bonds and a higher minimum wage. To build community resilience and ensure health equity in future public health crises, we need bold policy measures and serious commitment from government leaders to reducing social and economic inequality experienced by Black and Latinx populations.
Photo via Getty Images




