Understanding Mental Health Among Rural Populations
Cultural variations among Black and White rural populations deeply and uniquely impact their perceptions of mental health.

Read Time: 5 minutes
Published:
Decades of research indicates that the 46 million people who live in rural parts of the United States are more likely to be sicker and die earlier than their urban peers. What can we do to reduce this disparity? Primarily, we should address the structural barriers that can inhibit health for rural residents. We must also examine how cultural and social characteristics within rural communities can affect the health of the people who live there.
Many publicly available reports on rural health do not discuss the racial diversity of rural populations. Because of this, we know little about how members of different racial groups are impacted by rural health disparities. Race is a social construct. This means that societies have categorized people based on physical features like skin tone or hair type. Racial groups are not based on biological differences. Racial categories also change over time and can differ by culture and country.
Sometimes one racial group experiences relatively better or worse health than another racial group. These disparities in health outcomes can occur because of the ways that social conditions uniquely affect racial groups. For example, racism is a likely reason why Black Americans have higher rates of mortality from certain cancers than White Americans, despite similar incidence rates. Evidence suggests that racism is a root cause of the reason why Black, Indigenous, and other people of color typically experience worse physical health than White Americans. But, is this still true in rural communities where all racial groups can experience barriers to health?
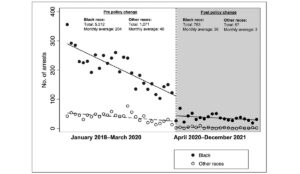
Interestingly, my team’s prior research on mental health indicates that living in a rural area is associated with worse mental health for White people and better mental health for Black people. This is puzzling. Could it be related to something called the “Black-White mental health paradox”? Researchers are interested in this “paradox” because White Americans do not endure the harmful psychological effects of racism but they typically have higher rates of depression and anxiety than Black Americans. My colleagues and I were curious if this Black-White mental health paradox would play out in rural communities where all residents typically have less access to mental health resources.
[C]ultural variations among Black and White rural populations can uniquely impact their perceptions of mental health.
To understand more about health and mental health in diverse rural communities, historians and health researchers invited 29 Black and White rural adults to tell their life stories in the format of an oral history. During this type of interview, rural residents talked about their health and discussed life in their community. My public health colleagues and I used systematic qualitative research methods to analyze their stories. Our goal was to highlight how these Black and White rural residents spoke about mental health and well-being.
We found telling nuances in how the interviewees described mental illness, stressors, and coping. There was consistent racial (but not gender or age) variation in how these rural residents characterized each topic. Rural White adults’ beliefs about mental illness were rooted in assumptions about the benefits of “hard work” and individual effort. For example, many said that people are personally responsible for depression, and should be able to overcome mental illness on their own. In contrast, Black adults described how events beyond one’s individual control can contribute to mental illness.
Stressors also differed along racial lines. For instance, White rural residents were concerned by their perception of social changes. They worried about “outsiders” moving into their community. Black rural residents tended to focus on past and present experiences of racism. Related to coping, the Black and White interviewees frequently talked about the benefits of being involved in religious organizations and having a “church community.” Additionally, all Black adults and one White adult described the value of having a personal relationship with God as a helpful way to manage stress.
Our findings suggest that cultural beliefs about work ethic and individualism could be important topics for future research on mental health among Black and White rural residents. Also, researchers and health care providers could consider how specific religious beliefs and practices relate to mental health in rural communities. Religion is not necessarily a culturally important factor for all Black or White Americans, but it could be helpful for health researchers to examine how religious components can affect mental health care-seeking behaviors among diverse rural residents.
These rural residents’ stories do not represent the perspectives of all people who live in rural communities. However, their stories convey that cultural variations among Black and White rural populations can uniquely impact their perceptions of mental health. Culturally appropriate public health messaging that speaks to the specific beliefs and attitudes of diverse rural populations could help us develop more effective interventions. We can potentially improve and support mental health in rural areas if we consider the unique cultural characteristics that exist within rural populations.