Telemental Health
Those with mental health challenges living in rural areas have long been at a significant disadvantage when it comes to receiving care due to lack of professional caregivers. Advances in technology such as live video teleconferencing have the potential to change this.

Read Time: 3 minutes
Published:
Those with mental health challenges living in rural areas have long been at a significant disadvantage when it comes to receiving care because, more often than not, there are not enough professionals. Advances in technology such as live video teleconferencing have the potential to change this. In the field of mental health, telemedicine has become an increasingly promising way to get psychological treatment to those in need .
Telemental health treatment is known by many names, including web-based treatment, digital interventions, e-therapy, and Internet-delivered cognitive-behavioral therapy (ICBT). Research has found positive results associated with anxiety, mood, and somatic disorders in terms of overall effectiveness as well as cost-effectiveness.
It is not surprising, then, that recent research from Harvard Medical School researcher Dr. Ateev Mehrotra and colleagues shows that the use of “telemedicine” has grown substantially in only a decade. From 2004 to 2014, usage grew from nearly 2,400 visits each year to about 87,000 visits each year—which amounts to an annual growth rate of 45.1%.
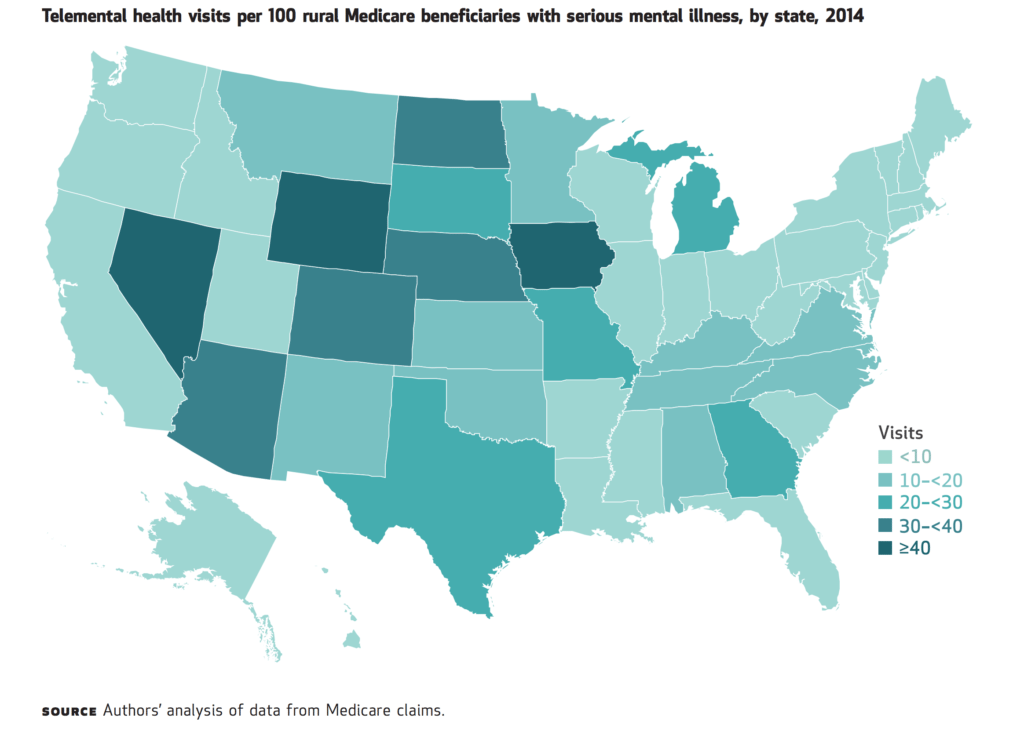
However, as the map above shows, telemental healthcare visits vary greatly among states, from less than 10 visits per 100 rural Medicare beneficiaries in some states to over 40 visits in others.

The research team attributed some of the variation to “payment and regulatory factors.” In other words, states that had passed parity laws made it easier for those covered by Medicare to receive telemental health care and, at the same time, for clinicians to be reimbursed for providing the services.
Changing Medicare policy to include telemedicine services has become a fairly recent subject of debate in Congress. Striking the right balance of telemental health usage will likely prove challenging. To increase coverage, certain proposed bills would allow for services to be provided in a patients’ home, rather than a host clinician’s office as is currently required. Current regulations also require that patients live in rural areas to be eligible for coverage; suggested expansions would allow for both rural and urban patients to receive telemedical services.
The authors of the study point out that an overuse of telemedicine could lead to the spread of low-value care—more convenience but lower quality. Given that usage is highly concentrated in certain areas and still only used by a small percentage of rural mental health care patients, this scenario seems a long way off. In the meantime, it will be important to focus on spreading the benefits of this technology to those most isolated and struggling with mental health challenges around the country.
Feature image: Alex Steffler, Rural Post, Outside Shafter, TX in Presido County. Just after sunrise along Highway 67 heading south from Marfa to Presidio, used under CC BY-NC 2.0