Three Notes on the Opioid Crisis
The opioid epidemic is the greatest American health crisis of this century. We think three areas receive far less attention than they should.
Read Time: 5 minutes
Published:

Three Notes on the Opioid Crisis
We are in the midst of the greatest American health crisis of this young century, an opioid epidemic that has now led to an astounding 500,000 deaths in the past two decades. There has been substantial ink—appropriately—devoted to this issue, we think there are three areas that receive far less attention than they should. One relates to the silent, concurrent increase in other substance use that is happening, the second relates to who we believe is affected by opioids, and the third to our best hope of stemming this crisis.
First, there are two other drugs being misused in America at newly alarming rates that have paralleled the rise in opioids. These are cocaine and its stimulant cousins that are prescribed, such as Adderall and Ritalin.
The availability of cocaine has risen, and with it there has been a 60% rise in cocaine overdose deaths in the past five years. Like opioids, cocaine addiction is a chronic relapsing condition that requires repeated treatment interventions. But unlike the treatments for opioids, which are effective in reducing deaths, the treatments for cocaine have extremely modest effects. With fentanyl now getting mixed into cocaine batches, even occasional cocaine use has become notably lethal.
In parallel, with increases in prescriptions of attention-deficit hyperactivity disorder (ADHD) medications of more than 50% in the past decade, there is an accompanying increase in the non-medical use of prescription stimulants. Stimulants are now the second most common drug misused on college campuses after marijuana, with 15-35% of college students having tried them recreationally—to study longer, concentrate better, get high, or lose weight—with ill effects on mood and sleep and an increasing potential for addiction.
Our second side note relates to who is being affected by opioids. This opioid tsunami has given us countless news stories about the toll on White, middle class, suburban, and rural users. While there have indeed been dramatic increases in opioid deaths in these groups, Black American deaths due to opioids have doubled in the past fifteen years. In some states, Blacks are experiencing opioid-related deaths at higher rates than other racial or ethnic groups. We must remind ourselves this is not only a White epidemic. While nationally the rate of opioid medication treatment is higher among Blacks who seek care than among other groups, rates of treatment remain low overall.
Finally, because access to treatment remains fragile, we should keep in mind that Medicaid remains a key source of coverage for many people who use drugs. As we ratchet up a treatment system for opioid, cocaine, and stimulant misuse that has been woefully inadequate, threats to Medicaid’s structure and funding need ongoing public health attention or the consequences of drug use will continue to expand.
Warmly,
Michael Stein & Sandro Galea

COMMUNITY WEALTH, COMMUNITY HEALTH
Each year, the County Health Rankings rate the health outcomes of each county in the United States. Using the data from these County Health Rankings, the authors of this study on wealth and health outcomes examined the assumption that lower-income counties perform worse than wealthier ones. They found that wealthier communities performed better but more than a quarter of those counties performed far better than wealth alone would suggest. Further, each additional percentage point of total public spending allocated toward community health care and public health increased the chances of a county being an over-performer by 3.7%. Community wealth correlates with health, but not always. Shifting spending to certain social services may positively impact population health.
CHANGING TOBACCO CULTURE
More than 58 million non-smokers are exposed to second-hand smoke. The Smoke Free Homes program, consisting of three mailings and a single counseling telephone call, was implemented in smoking-discordant households (≥1 smoker and ≥1 non-smoker) in Texas to protect non-smokers. Working in partnership with 2-1-1 social services information and referral systems, these authors report on a randomized controlled trial that enrolled 508 primarily low-income, African American women. At six months, 63% of the intervention participants self-reported smoke-free homes vs. 38% of control participants. The goal of this low intensity program targets reduced exposure to smoke rather than smoking cessation, and could be extended to federally-subsidized housing.

PLANNING FOR END-OF-LIFE
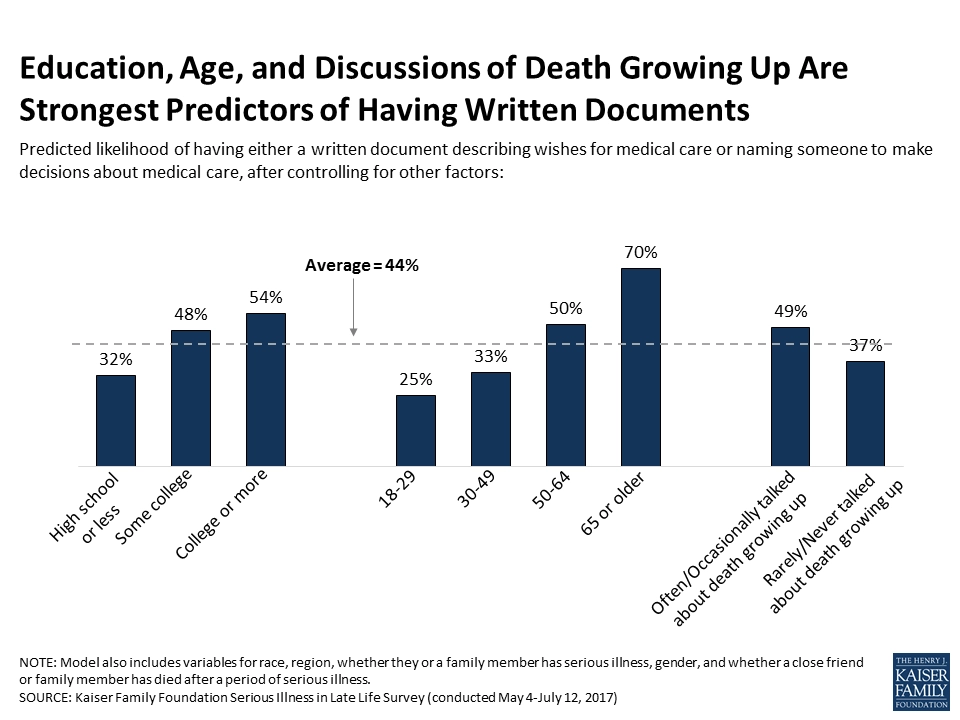
Results of a recent survey show that older adults are more likely than younger people to have documented their end-of-life wishes. Despite this, few adults with or without written documents discussed end-of-life care with their doctors.
The figure above shows that on average, those surveyed had a 44% likelihood of having a written plan or could identify someone to make decisions about their end-of-life care. Age, education, and discussions about death are predictors of having such a plan. Those with a college education or higher were most likely to have a written document, compared to those with some college, high school, or less education. Also, talking about death while growing up correlated to having written documents about wishes for end-of-life care.
In addition, adults aged 65 or older were most likely to have a written document or to name someone to take charge of their medical decisions. Although older adults are more likely to have some end-of-life plan, the survey found that seriously ill older adults are less likely than their healthier counterparts to report having written documents. This is linked to seriously ill people reporting lower education levels, which the above figure depicts as being a strong predictor of not having a written plan for end-of-life.
Care settings encouraging or mandating doctors to use an advanced directive toolkit, like the one created by the National Physician Orders for Life-Sustaining Treatment Paradigm, can improve the communication gap, and help seriously ill patients better express their wishes for end-of-life care.
Graph: Kaiser Family Foundation, Serious Illness in Late Life: The Public’s Views and Experiences, Section 3: Documenting and Talking about Wishes, Figure 31: Education, Age, and Discussions of Death Growing Up Are Strongest Predictors of Having Written Documents, Bianca DiJulio, Liz Hamel, Bryan Wu, and Mollyann Brodie




