Dosing Hope: Exploring Psilocybin for Patients Facing Mortality
Psilocybin therapy may help ease end-of-life dread, but broader acceptance requires better patient education and clinician training.

Read Time: 2 minutes
Published:
Facing death often triggers overwhelming fear and dread, especially in quiet moments without work or companionship to distract the mind. For people receiving palliative care, specialized treatment for serious, complex, and often terminal illnesses, this emotional toll is a familiar reality. Palliative care focuses on managing pain and symptoms to improve quality of life and can begin at any stage of illness.
People receiving palliative care may find themselves grappling with existential questions about the purpose and shortness of life, their achievements, and regrets. For some, these thoughts can evoke depression, anxiety, and a profound sense of hopelessness. Sleep and appetite may be disrupted, leading to fatigue, weight loss, and overall decline in physical function.
Health care providers often struggle to ease the psychological distress that can come with palliative care. Recently, psilocybin, the active compound in psychedelic mushrooms, has emerged as a potential solution. Although psychedelic research is advancing, negative perceptions continue to hinder conversations and understanding of their possible therapeutic benefits.
Julia Ruixi Wang and coauthors surveyed palliative care patients to explore their attitudes toward using psilocybin to treat existential distress. The survey assessed patients’ knowledge, concerns, and interest in psilocybin therapy.
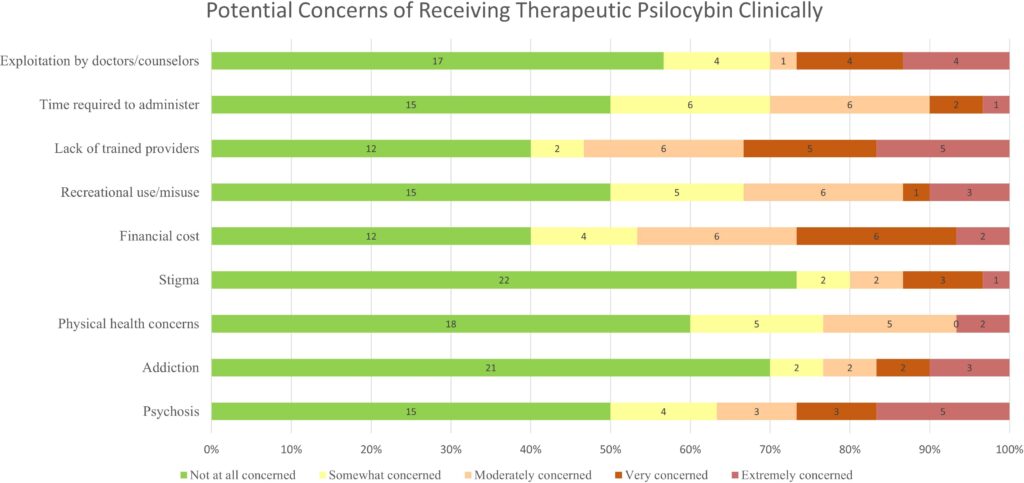
Overall, most participants (51.6%) expressed interest in psilocybin therapy, while 32.3% were not interested. The top concerns included risk of psychosis (16.1%), lack of trained providers (16.1%), and potential exploitation by medical professionals (12.9%). Most participants were least concerned about stigma or addiction.
Few participants reported having strong knowledge of psilocybin. Only 9.7% said they understood its therapeutic use, and 16.1% were aware of risks and side effects. Most people’s knowledge came from personal experience, friends, or the media. Trusted sources for learning included doctors and other researchers.
Concerns did not significantly affect participants’ interest in psilocybin therapy. However, opinions were clearly divided: 22.6% strongly agreed with receiving psilocybin therapy, while 25.8% strongly disagreed. Interest was not tied to any demographic factors, though more data is needed for confirmation.
Psilocybin’s euphoric and “mystical” effects may help ease end-of-life dread, but they can also have negative side effects, which have made legalization controversial. Psychedelics have been legalized for therapeutic use in two states, and research is now supported in seven. To better understand the potential of psychedelic therapy in palliative care, future efforts must focus on patient education, clinician training, and the development of safeguards.



