Criminalizing Pregnancy
Criminalizing substance use during pregnancy is common, but there is no evidence that prosecuting women for using substances during pregnancy helps.

Read Time: 4 minutes
Published:
Substance use during pregnancy is an important public health problem. Approximately 380,000 babies are born to women who use illicit drugs. Drug use during pregnancy increases the risk of adverse maternal and neonatal outcomes such as maternal fatalities, prolonged hospital stays, fetal alcohol syndrome, neonatal abstinence syndrome, and poor fetal growth‒including low birth weight. The cost of treating neonatal drug withdrawl in 2014 alone was $462 million.
In February, the state of Tennessee tried to re-prosecute women whose babies were born harmed or addicted to drugs by renewing its 2014 assault statute (HB 1168). The bill would have authorized the prosecution of women with pregnancy complications due to the illegal use of narcotic drugs such as OxyContin, Vicodin, codeine, morphine, methadone, and fentanyl. The proposed legislation died this spring after receiving enormous attention from media reporting its potential jeopardies.
Criminalizing substance use during pregnancy is common in the US. Twenty-three states plus the District of Colombia have taken a punitive approach responding to the rising need to treat pregnant women for substance use. State policies allow the judgment of substance use during pregnancy to be child abuse and use civil commitment statutes to detain women. Additionally, 25 states and the District of Columbia mandate health care professionals to report suspected prenatal drug use or inform professionals to test for prenatal drug exposure if they suspect drug use. Some state Medicaid programs have pre-authorization policies for medication-assisted treatment against opioid use disorder.
Such laws have a minimal effect on reducing the number of babies born addicted to or harmed by narcotics. And they may drive pregnant women who have opioid use disorder to avoid prenatal care and addiction treatment due to the fear of being arrested during pregnancy. Without adequate care, pregnant women with substance use disorder are less likely to have a healthy pregnancy and baby.
There has never been a more fundamental time to invest in prevention and treatment for a vulnerable population like pregnant women.
There is no evidence that prosecuting women for using substances during pregnancy helps mothers or babies. Such prosecution has increased the inequity among minorities and socioeconomically disadvantaged women. The criminalization of addiction prevails despite the medical standpoint that a chronic medical disorder can be treated and managed. The criminalization of drug use has been increasing as it perpetuates stigma, and individuals in recovery are still being blamed for their disease.
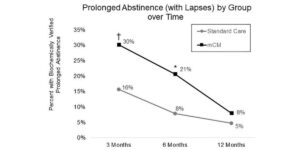
The good news is that 18 states have “carrot” policies that increase access to state-funded drug treatment programs by targeting pregnant women to facilitate admissions. Ten states prohibit treatment programs from discriminating against pregnant women. For example, Colorado encourages health care practitioners to refer women for a needs assessment if they deem that patients are at risk of poor birth outcomes due to substance use.
Pharmacotherapy treatment is standard care for treating pregnant women who have opioid use disorder because detoxification during pregnancy increases the likelihood of seizures during withdrawal and it puts both the mother and fetus at risk. Medication for opioid use disorder, such as methadone and buprenorphine, treats opioid addiction and decreases adverse outcomes in pregnant women and their babies. Yet, access to treatment remains low. Only 36% of the substance use disorder treatment facilities offer medication for opioid use disorder.
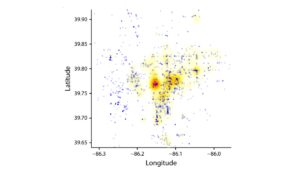
Pregnancy is an opportunity for women who have a substance use disorder to seek and receive drug treatment. Efforts are being made at multiple levels of the healthcare system to aid the process. The Centers for Medicare and Medicaid Services recently announced a grant opportunity to coordinate care and integrate services for pregnant women and babies on Medicaid who are born with neonatal abstinence syndrome. Community-level interventions also exist.
There has never been a more fundamental time to invest in prevention and treatment for a vulnerable population like pregnant women. States should propose bills that can increase access to treatment services for this marginalized and vulnerable group and not deter them from accessing treatment.