Trust or Treat? Antibiotic Misuse
Individuals with high levels of medical mistrust were 3.2 times more likely to use non-prescription antibiotics than those with low levels of mistrust.

Read Time: 2 minutes
Published:
The discovery of antibiotics represents one of the greatest public health achievements in the 20th century. They continue to save millions of lives every year. However, these medications are at risk of losing their effectiveness.
Antibiotic resistance occurs when harmful bacteria continue to cause infections despite the use of antibiotics because those medications no longer work. Over-prescription and misuse of antibiotics has caused antibiotic resistance. In the U.S., 2.8 million antibiotic-resistant infections occur each year, resulting in over 35,000 deaths. If antibiotics can no longer treat infectious diseases, public health is threatened.
Programs have been developed to promote the appropriate use of antibiotics to combat antibiotic resistance. Such initiatives are implemented in health care settings, targeting clinicians who often prescribe antibiotics unnecessarily. However, these programs assume that people are receiving their antibiotics in the clinical setting. Yet many people choose to self-treat illnesses. One reason for this self-treatment is thought to be medical mistrust, which is associated with fewer interactions with health services.
Brooke A. Hawkes and colleagues evaluated the potential correlation between medical mistrust and non-prescription antibiotic use. They used an online survey to measure levels of distrust in the medical system and usage of non-prescription antibiotic use in adults living in the U.S./Mexico border region.
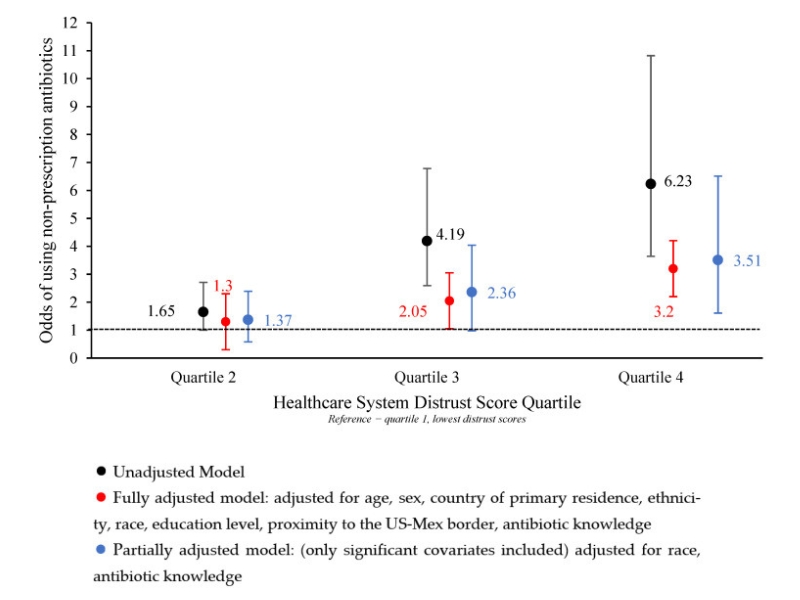
The figure above shows how likely someone is to use non-prescription antibiotics based on their level of distrust in the health care system. Quartile 2 indicates the least distrust and Quartile 4 represents the highest distrust. Researchers found that individuals with high levels of distrust were 3.2 times more likely (red vertical bar in Quartile 4) to use non-prescription antibiotics than those with low levels of distrust.
The researchers suggest that proper antibiotic use programs should be expanded outside of the clinical setting to the community, to better address self-treaters. Community-based programs can teach those outside of the health care setting why limiting antibiotic use is critical in the fight against antimicrobial resistance.
Databyte via Brooke A. Hawkes, Sana M. Khan, Melanie L. Bell, et al. Healthcare System Distrust and Non-Prescription Antibiotic Use: A Cross-Sectional Survey of Adult Antibiotic Users. Antibiotics, 2023.



