The Illusion of Clinical Success
Clinicians are responsible for fixing the immediate health problem, but must eventually also grapple with the underlying concerns.
Read Time: 5 minutes
Published:

The Illusion of Clinical Success
As doctors we have both had our fair share of patient success stories. A patient presents herself to our office or emergency room with a problem, we diagnose it, prescribe treatment, and the patient gets better. We can remember Lois who presented with vomiting, whom we diagnosed with gastroenteritis, treated and restored to health two weeks later. And Emmanuel who came to the emergency department with a cut on his forehead because he fell down the stairs. He was sutured up and the cut healed nicely. All clinicians have these stories. They are the reason why many of us went to medical school, to heal people, to make them better.
And yet, anyone who has worked as a clinician knows what often happens next. The patient who had gastroenteritis returns again a few months later, this time with shortness of breath that turns out to be influenza pneumonia. The patient who had the cut on his forehead returns this time with hepatitis. The reason for this, of course, is that both had common causes that were not dealt with when we, the physicians, dealt with the presenting complaint. Yes, the immediate concern was gastroenteritis, but the root cause was a refrigerator that went out when the electric bill wasn’t paid that resulted in contaminated food. That same root cause—poor living conditions—resulted in pneumonia transmitted from another unvaccinated resident in a densely populated house. For the patient who presented with a fall and a cut, and later hepatitis, his medical problems were all related to alcohol dependence that had its roots in adolescence.
These observations are all immediately recognizable to clinicians who struggle to identify and treat a root cause whose sources are often outside the medical system. And that is what makes root causes so powerful: they escape ready treatment and underlie a multiplicity of medical presentations. The same root cause can be responsible for a gastrointestinal or a respiratory problem, for an injury or a hepatic problem. This is why when we think of the causes of medical problems strictly from an organ-based perspective it is never enough. Because medical problems often do not arise in their end-organs; they are bodily manifestations of underlying issues.
What does this mean for the role of the clinician? Clinicians remain responsible for fixing the immediate problem, but must, we believe, eventually also grapple with the underlying concerns. The issues of inadequate housing, limited access to addiction treatment, poverty, and terrible neighborhoods are medical problems. But they are larger than any individual clinician caring for an individual patient. Clinicians can choose to be advocates themselves, voices for public health outside of the hospital or clinic, or they can advocate that their hospital or clinic embrace these issues with fervor. Absent that, our clinical success remains fleeting, illusory.
Warmly,
Michael Stein & Sandro Galea

EARLY OFFENSES REQUIRE EARLY ACTION
For two decades, these authors have collected data about approximately 100,000 pre- and early adolescents referred to the South Carolina Department of Juvenile Justice, and a control group of 100,000 non-delinquents of similar gender, ethnic composition, and birth year. This summary announces three factors associated with criminal justice system recidivism. First, prosecution of youth for less serious crimes tends to be associated with higher likelihood of additional offenses, especially when the youth shows limited pre-offense problem behavior. In more serious cases, failure to prosecute is more often associated with re-offending. Second, preventing the first offense is critical and requires interventions that support the parents and family. Intervention is important during the preschool period, when disruptive behaviors often related to mental health problems and child maltreatment can be clearly noted. Third, school-based interventions focused on changeable risk factors (e.g., low skills, substance misuse, defiant behavior) are critical. Targeting high-risk individuals early can result in high savings. Diverting a 14-year-old high-risk juvenile from repeated crimes can result in savings between $2.6 and $5.3 million over their lifetime and prevent consigning a young person to the revolving doors of the justice system.

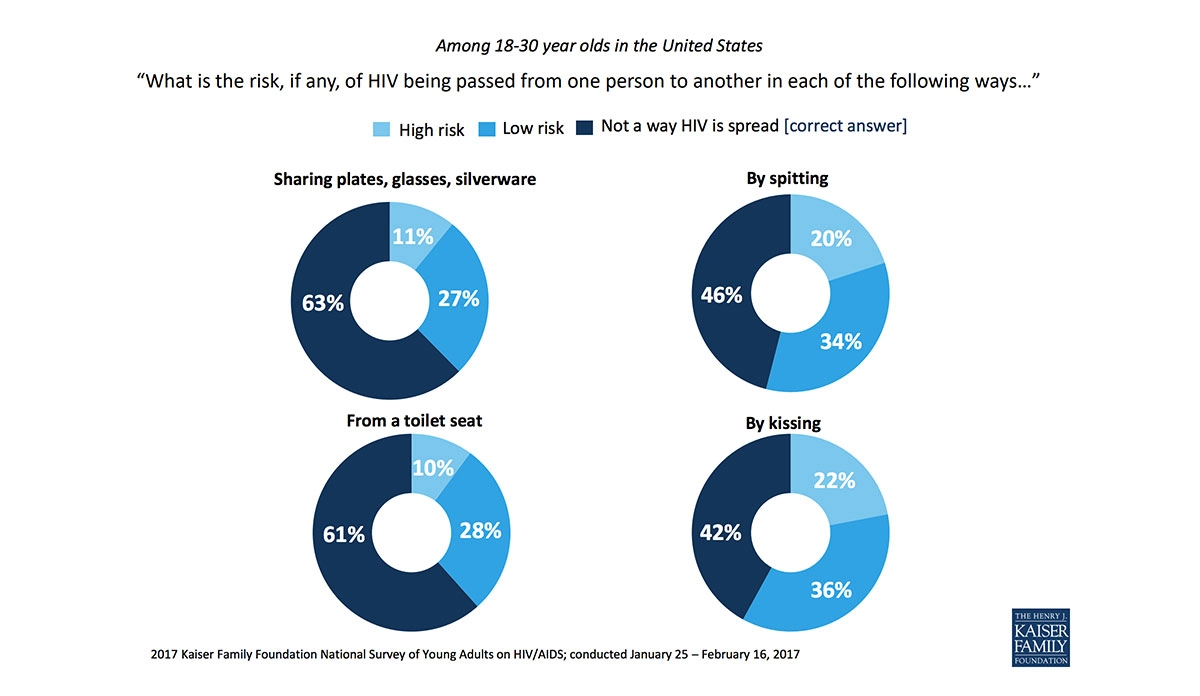
HIV FROM SILVERWARE? FORK NO!
In 1983, the Centers for Disease Control and Prevention identified the main ways that HIV is transmitted, as well as ways that it is not, publishing this information in the Morbidity and Mortality Weekly Report. Even though this information has been widely available for over three decades, misperceptions about HIV transmission persist.
The Kaiser Family Foundation National Survey of Young Adults on HIV/AIDS included results from nearly 1,800 people between the ages of 18 and 30 years. Interviews were in English and completed either online or by telephone. The graphic shows young Americans’ answers.
A large number of respondents did not know how one becomes infected with HIV. More than one-third of survey respondents believe the virus can be spread through sharing kitchenware (plates, glasses, and silverware) and from a toilet seat. Over half of the survey respondents thought spitting and kissing were ways HIV could be spread. HIV cannot be spread through any of these methods.
These misperceptions contribute to the stigma that HIV-positive individuals continue to face. In the same survey, over half of the respondents reported that they would be uncomfortable having an HIV-positive roommate (51%) or having an HIV-positive individual prepare their food (58%).—Chrissy Packtor, PHP Fellow
Graphic from Kaiser Family Foundation 2017 National Survey of Young Adults on HIV/AIDS chart pack