The Caregivers Holding Up America’s Health System
The Trump administration’s restrictive immigration policies are destabilizing a health care workforce the country cannot afford to lose.

Read Time: 4 minutes
Published:
America’s aging population is growing, but the health care system doesn’t have the workforce to support it. Long-term care facilities are already struggling. Nearly half of U.S. nursing homes turn away new residents because they are understaffed. And only 19% currently meet the federal minimum staffing standards that will be required by Medicare and Medicaid in 2029.
As a result, older adults wait longer for basic assistance, face increased risks of falls and infections, and experience more frequent hospitalizations. With the demand for elder care expected to surge in the next decade, the shortage of workers is reshaping where and how elderly Americans receive care—often pushing them to rely on relatives and home health workers to care for them at home or in senior living communities. Such informal care has become a necessary but often inadequate alternative to institutional care.
Yet the people providing care at home often face precarious working conditions. Most home care workers are underpaid, making retention a constant challenge. About 18% of the health care workforce is made up of immigrants, who play an especially vital role in nursing homes and home care agencies. They take on difficult shifts, provide culturally responsive care, and form the backbone of a system already stretched thin. Without them, the system loses both capacity and quality.
But now, the Trump administration’s renewed push for restrictive immigration policies could further destabilize this already fragile sector. The president’s efforts to deport undocumented immigrants, end Temporary Protected Status for workers from Venezuela, Haiti, and Afghanistan, and implement stricter caps on legal immigration all threaten to displace vital health care workers.
The Trump administration’s restrictive immigration policies are destabilizing a health care workforce the country can’t afford to lose.
These policy changes raise urgent questions about the future of the health care workforce. Just how many workers, especially those supporting elderly patients, could be affected?
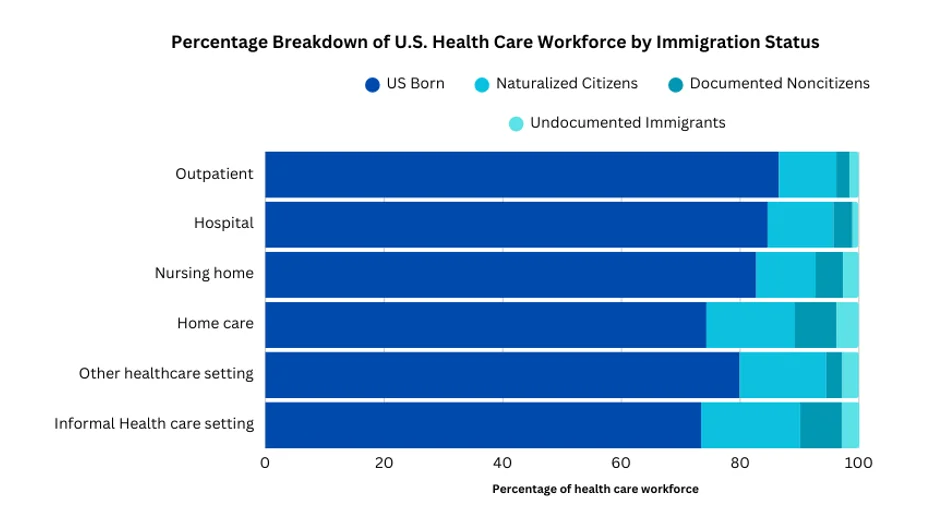
New research by Lenore Azaroff and colleagues breaks down the numbers to show what’s at stake. The team used data from the 2024 Current Population Survey, administered by the U.S. Census Bureau and Bureau of Labor Statistics, to calculate the citizenship and documentation status of people employed in different health industries.
As of March 2024, the U.S. health care workforce included more than 2 million naturalized citizens and 1 million documented and undocumented immigrants. Depending on the specific health care setting, people born outside the U.S. represent between 14% and 27% of the workforce. Roughly 10% of people working in home care agencies and informal health care settings, and 7% of those working in nursing homes, are non-citizens. Additionally, there are more than 360,000 undocumented people and 160,000 non-citizens from countries with Temporary Protected Status who work in health care. All of these workers are at greater risk under the country’s new immigration policies.
Given the current staffing shortages, there simply aren’t enough native U.S. citizens qualified or willing to fill all the additional positions that would become vacant if immigrants are pushed out of these jobs. And it’s not just today’s workforce that is at risk—the 2.3 million naturalized citizens who are currently physicians, nurses, aids, and other health workers were once immigrants, as well. Tighter immigration restrictions threaten both current staffing and the pipeline of future care providers.
The Trump administration’s restrictive immigration policies are destabilizing a health care workforce the country can’t afford to lose. Deportations and newly imposed legal barriers to immigration risk destabilizing the health care system, delaying hospital discharges, overcrowding emergency departments, and straining clinical staff. The study authors warn that these policies risk undermining care not just for older Americans, but for everyone who depends on a functioning health system.



