Surgery Can't Wait: A Crisis in Rural America
Rural patients must travel longer distances to hospitals for emergency surgery, and quality of care and affordability are not guaranteed.

Read Time: 2 minutes
Published:
Delaying surgery isn’t just an inconvenience—it’s a serious health risk. Without timely surgical care, even a common issue like appendicitis can lead to a ruptured organ, dangerous infection, or death. Yet for nearly 1 in 3 Americans, getting an appendectomy or similar emergency procedure is a major challenge.
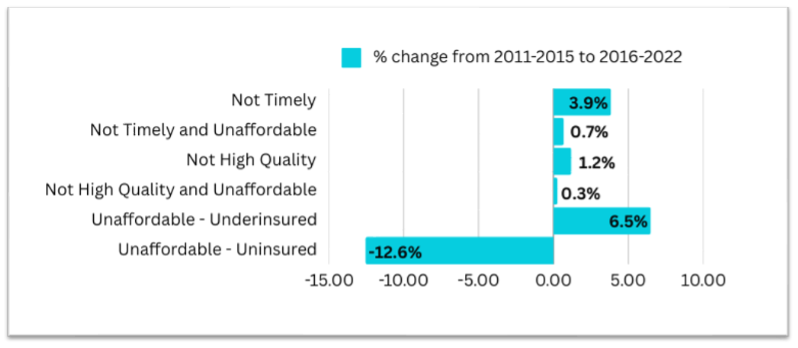
In a recent study, Cody Lendon Mullens and colleagues compared access to emergency surgery from 2011-2015 and 2016-2020 by analyzing data from the American Hospital Association, Medicare, and Medicaid. They found that, over the past decade, the percentage of Americans unable to access timely, high-quality, and affordable surgery remained the same—around 30%. What did change, though, were the reasons behind the lack of access.
From 2011 to 2020, the number of people who couldn’t access emergency surgery due to being uninsured decreased by 12.6%—likely the result of the Affordable Care Act, which has insured 50 million Americans since 2014. However, as health care costs continue to rise, affordability remains the most significant barrier. Mullens’ study showed that many who were once uninsured are now underinsured, meaning they have insurance but still cannot afford care.
Others who were once uninsured now face a new, growing challenge: delays. From 2016-2020, the number of Americans who lived more than a 60-minute drive from a hospital offering emergency surgery rose by 3.9%, or 4 million people, compared to the previous five years.
In rural America, longer travel distances are expected, but over 150 rural hospitals have closed since 2010, making geographic barriers worse. Patients must now travel farther, and staff and resources at the remaining hospitals are stretched to their limits. The shortage of surgeons in rural areas also undermines the quality of care.
Mullens and colleagues highlight the harsh reality that being insured does not guarantee surgical care when needed, especially in rural areas. However, surgery can be made more accessible through targeted interventions. Financial incentives to attract surgeons to underserved areas, investments in rural health care infrastructure, and expanded telemedicine for pre- and post-operative care can play a crucial role in improving access and health.