Police and the Public's Health
Police work is community work. Performed on the street, in public settings and private homes, police work shapes the health context of cities and neighborhoods, and affects the lives and behaviors of countless citizens.
Read Time: 5 minutes
Published:

Police and the Public’s Health
Police work is community work. Performed on the street, in public settings and private homes, police work shapes the health context of cities and neighborhoods, and affects the lives and behaviors of countless citizens. While there has been much concern in recent years—appropriately—about how some police activity has harmed health, particularly among minority communities, it is worth focusing on the potential for police work to improve the health of the public.
Most police interaction with the public does not involve major crimes or violence that requires arrest or use of force. Police beat work is filled with low intensity interactions in which officers serve as problem‐solvers. We think of this as public health work; police are one of the forces that generate health in many places.
Police often find themselves at the center of our national public health crises. They are first responders to opioid overdoses; they intercede in intimate partner violence; and they approach the homeless, three of the major public health challenges of our time. Efforts such as the Police Assisted Addiction and Recovery Initiative (PAARI) have been at the forefront of innovative approaches towards mitigating the opioid epidemic.
One of the central challenges faced by police officers in this country is ongoing interactions with people with mental illness. One in ten police contacts with the public in the US involves persons with serious mental illnesses. Police officers are trained in self defense and most often think in terms of force and arrest. Yet officers now commonly transport people to hospital emergency departments for psychiatric evaluation rather than to jail. In the field, officers must be creative and persuasive to avoid unnecessary arrests.
Increasingly, large cities are developing Crisis Intervention Teams (CIT) to improve safety and divert individuals from criminal justice involvement. Crisis Intervention Team training involves learning the signs and symptoms of mental illness and the threats posed, spending time with mentally ill persons, their families and mental health service providers, and learning new tactics of negotiation and skills in decision-making.
In places where CIT takes hold, police officers do preventive work—they engage families, they manage complex mental health needs. Police serve a role as front line public health workers, linking individuals to treatment and other resources that can inflect the trajectory of a person’s life for the good.
CIT training is currently voluntary (and selective) in a limited number of police forces. Disseminated more widely, such training can support a cultural shift toward improved de-escalation and diversion practices in law enforcement. Such an investment of police time and resources could have powerful consequences on the public health of communities.
Warmly,
Michael Stein & Sandro Galea

MENTAL HEALTH BY APP
This qualitative study describes some common misconceptions that clinicians may have about their patients using Smartphone apps for mental health care. First, providers should resist assuming that older patients are not interested in incorporating mental health apps into their care. Clinicians should note, however, that smaller typeface and a touchscreen format may prove challenging or prohibitive for older patients with declining vision and dexterity. Second, many mental health apps can serve as helpful tools for those not receiving face-to-face mental health care. Patients may believe that mental health apps are an impersonal replacement for personal time with a therapist, but apps can serve as platforms to log thoughts, track symptoms, or receive psychoeducation between sessions. Finally, it is essential for patients to be fully informed on the extent of privacy provided by apps and the potential risks of logging personal information in an electronic format.

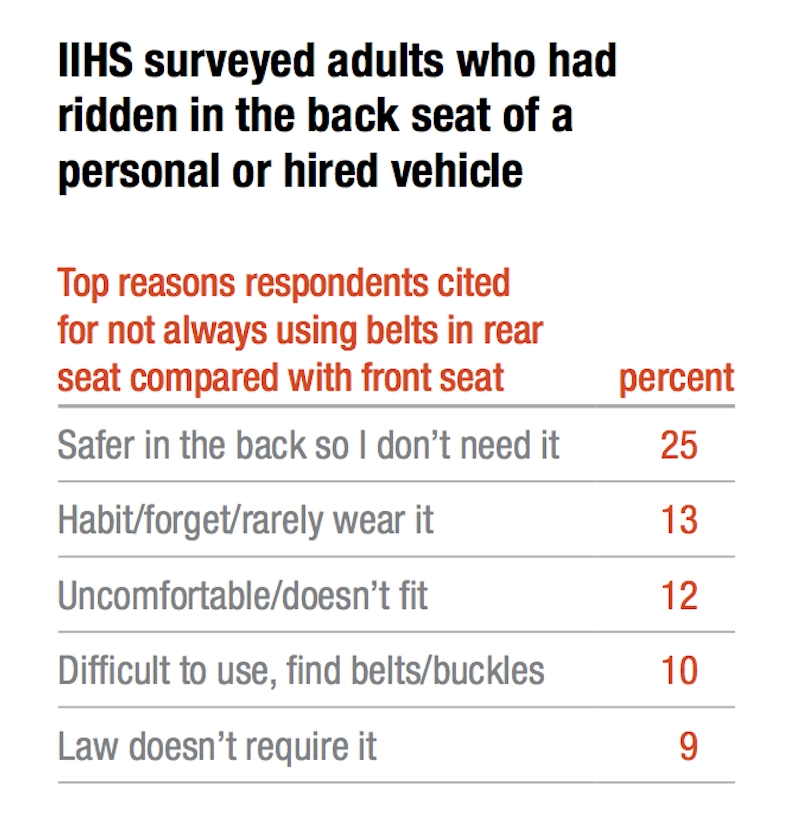
BUCKLE UP FOR SAFETY
Nearly half of the deaths from car crashes in the United States are due to not buckling up. An estimated 2,400 lives could have been saved in 2016 if drivers and passengers had fastened their seat belts.
Back seat passengers tend to buckle their belts less often than persons sitting in the front. An average of 11% fewer back seat passengers reported wearing a seat belt compared to front seat riders.
The data in the table come from a national survey conducted by the Insurance Institute for Highway Safety / Highway Loss Data Institute. The most common reason that back seat passengers decided not to wear a seat belt was because they felt safer sitting behind the driver.
Yet back seat passengers who do not strap in are eight times more likely to sustain a serious injury in a car accident. Failure to buckle up is not just a personal risk. Unbuckled passengers become projectiles in a crash, jeopardizing the safety of everyone in the car. Other car passengers are three times as likely to be fatally injured when a passenger behind them doesn’t buckle up.
Image: IIHS Status Report newsletter, Vol. 52, No. 5, August 3, 2017