Pharmacy Deserts Hinder Medications Access in Segregated Black and Latino Neighborhoods
Lacking access to a local pharmacy can directly impact health equity.
Read Time: 5 minutes
Published:
Pharmacies are an important part of the health care system because they dispense prescription and over-the-counter medications and increasingly provide preventative services, including Covid-19 testing and immunization. However, geographic access to pharmacies varies throughout the US, especially in segregated American cities. Disparities in pharmacy access impact medication adherence, or how well a patient takes their medications. And medication adherence influences health outcomes ranging from cancer progression to cardiovascular disease.
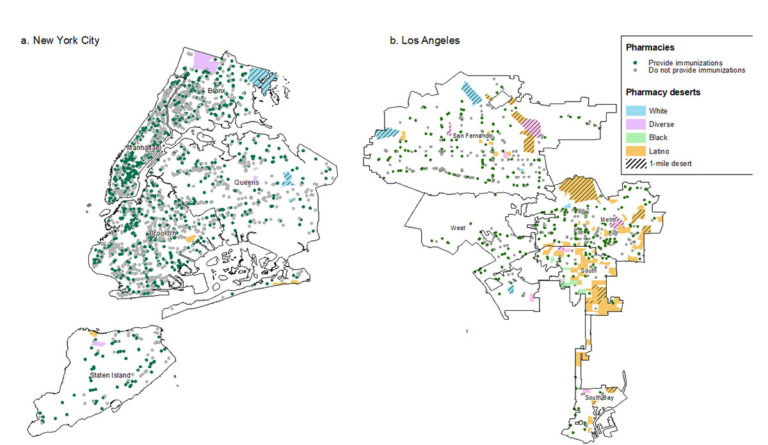
In May, we published findings from a study of pharmacy locations in US cities between 2007 and 2015. We found that one-in-three neighborhoods throughout the 30 largest cities in the United States are pharmacy deserts. We defined pharmacy desert as a neighborhood where: (1) the average distance to the nearest pharmacy was one mile more or (2) the average distance to the nearest pharmacy was at least half a mile and at least 100 households had no vehicle access. We found troubling, persistent disparities associated with neighborhood racial and ethnic composition. Nearly 40% of segregated Black and Latinx neighborhoods were deserts in comparison to one quarter of White neighborhoods.

In an updated study, we found that these disparities persisted in the four largest US cities through 2020 (figures above). Importantly, the few pharmacies that served segregated Black and Latinx neighborhoods were less likely to offer immunization, 24-hour availability, and drive-thru services than pharmacies located in other neighborhoods. They were also more likely to more likely to close permanently.
This inequitable distribution of pharmacies is not an accident. It is an expected result of longstanding health policies that neglect to protect pharmacies located in underserved neighborhoods. For example, many pharmacies close due to low reimbursement rates for Medicaid and Medicare Part-D (prescription drug benefits for older adults). Insurance plans often institute narrow pharmacy networks (which financially incentivize patients to use pharmacies through lower cost-sharing) that exclude many pharmacies in segregated communities of color.
Such policies are a form of structural racism that affects where pharmacies locate and stay open. For example, to improve the economic viability of pharmacies at risk of closures, 11 states provide higher Medicaid reimbursement rates in rural areas. However, most of these states fail to provide similar protections to pharmacies located in segregated Black and Latinx neighborhoods in their urban centers.
Low reimbursement rates are a root cause of pharmacy closures. Medicare and Medicaid programs must ensure that their reimbursement policies not exacerbate disparities across segregated neighborhoods. For example, the Centers for Medicare and Medicaid Services (CMS) could update Part D requirements and mandate higher reimbursement for pharmacies located in pharmacy deserts.
States could also require Medicaid managed-care plans to meet convenient pharmacy access standards. In other words, beneficiaries in cities should have access to in-network pharmacies within 1 mile of their home. Independent pharmacies are critically important because they disproportionally serve segregated minority neighborhoods, but they are more likely to close. Therefore, any policy reforms should guarantee that independent pharmacies, not just large chains, are included in Part D and Medicaid managed-care pharmacy networks.
In Chicago, an extremely segregated city, one of the largest providers of Medicaid managed-care, Aetna Better Health, narrowed its network of pharmacies to CVS pharmacies (the majority of which are in white neighborhoods) and a small number of independents. This reduced access to convenient pharmacies for Medicaid beneficiaries, who are disproportionately Black and Latinx. It may also lead to closures of pharmacies operating in segregated minority neighborhoods, as beneficiaries are forced to use pharmacies elsewhere. Residents of segregated Black neighborhoods were already experiencing substantial barriers to medication access, as at least 60 pharmacies operated in a reduced capacity in summer 2020 during the Black Lives Matter protests. Several closed and never reopened.
Lacking access to a local pharmacy can directly impact health equity. Pharmacy closures are more likely to occur in Black and Latinx neighborhoods and lead to lower adherence to medications that can prevent a heart attack or stroke. Inequitable access to pharmacy services, such as drive-thru and immunization, has likely aggravated disparities in COVID-19 testing and vaccinations in these same neighborhoods. Therefore, to improve health equity, we need to improve access to pharmacies and their services in Black and Latinx neighborhoods throughout the country.
Notes: The figures depict the geographic distribution of pharmacy deserts and the number of pharmacies that provide immunization services in each city (not to scale). Pharmacy deserts were those low-income neighborhoods (1) whose average distance to the nearest pharmacy was ≥1 mile or (2) whose average distance to the nearest pharmacy was ≥0.5 mile and at least 100 households had no vehicle access. We also delineate city subdivisions, including boroughs in New York Cities, service planning areas in Los Angeles, planning districts in Chicago, and council districts in Houston. Adapted from Guadamuz JS, Alexander GC, Kanter GP, Zenk S, Wilder JR, Qato DM. Access to Pharmacies and Pharmacy Services in New York City, Los Angeles, Chicago, and Houston, 2015-2020. J Am Pharm Assoc. 2021.
Disclosures: J.S. Guadamuz reported current employment with Flatiron Health Inc, an independent subsidiary of Roche. D.M. Qato does not report potential conflicts of interest.




