Mobile Clinics to Mitigate Emergent Care Gaps
During health emergencies, people with lower incomes and limited access to care were more likely to seek support at mobile clinics.

Read Time: 2 minutes
Published:
Timely medical care remains out of reach for millions of Americans. Barriers such as cost and transportation contribute to wide care gaps, including delayed treatment for chronic conditions and unequal vaccine coverage. These disparities become especially pronounced during public health emergencies, when demand for care surges and resources are stretched thin.
During the COVID-19 pandemic, low-income families and families of color faced higher risks of contracting the virus compared to higher-income and White families, respectively. Mobile clinics removed the need to travel long distances to receive care in many communities, helping ease the pandemic’s impact on rural communities, in particular.
Mobile clinics deliver medical care directly to communities with limited health care access, often at low or no cost. New research explored which populations rely most on mobile clinics during public health emergencies.
Lior Rennert and associates examined the usage rates of mobile health clinics from 2021 to 2022 in communities least equipped to handle public health emergencies and with the lowest vaccination rates. Six mobile clinics were deployed to 149 sites in South Carolina, administering over 12,000 COVID-19 vaccines to 8,545 individuals.
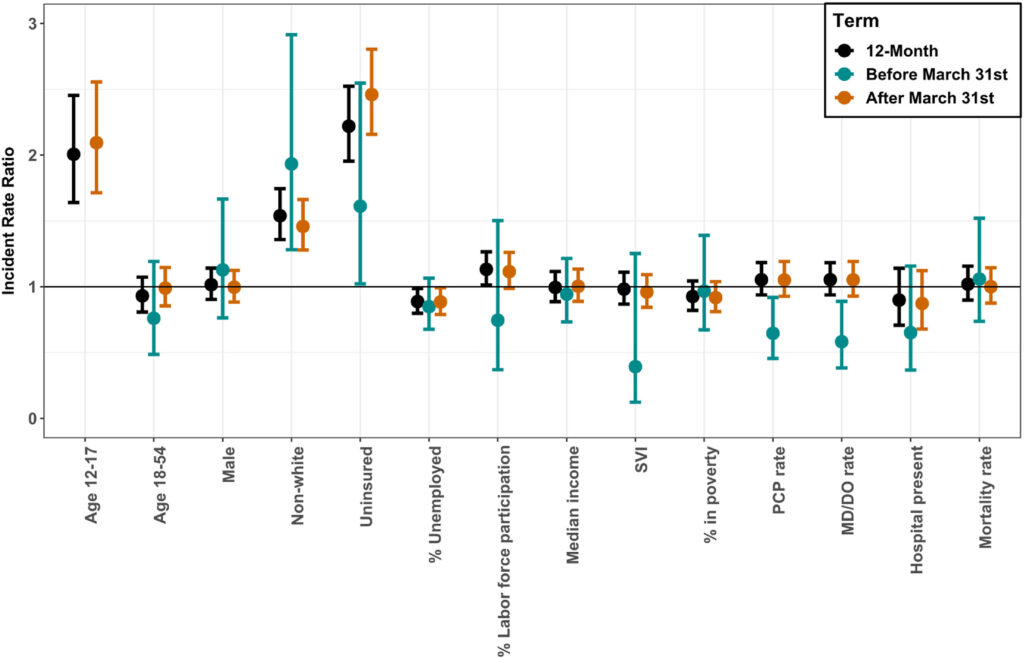
Over a 12-month period, Black, Hispanic, and uninsured individuals were more likely to receive vaccinations through mobile clinics than their White and insured counterparts. After vaccine eligibility expanded to those 16 and older on March 31, 2021, adolescents became more likely than older adults to use mobile clinics for vaccination. During the nationwide vaccine shortage, rural residents—who often face limited access to local doctors and hospitals—relied more heavily on mobile clinics for vaccine coverage due to reduced travel burden and convenience. Across all settings, schools and homeless shelters reported some of the highest vaccination rates.
The results reveal that lower income, limited access to care, and travel challenges are linked to increased mobile clinic use during emergencies. Identifying communities that benefit most from targeted mobile clinic deployment can strengthen emergency responses and ensure appropriate resource allocation.
Mobile clinics also serve as a powerful tool to reach socially disadvantaged communities beyond crises by providing routine exams and community surveillance. Thoughtful integration of these clinics into modern health infrastructure can expand care access, improve population health, and reduce the nation’s health care costs.



