Good, Bad, and Ugly
Local public health systems could play a significant role in reducing rural disparities during the Covid-19 pandemic and beyond.
Read Time: 2 minutes
Published:
Covid-19 has exposed the good, bad, and ugly of public health departments in our country. The pandemic has demonstrated just how important health departments are to our lives. Unfortunately, many of us came to this realization because critical services were slow, insufficient, or absent altogether. Public health workers throughout the country are quitting their jobs in droves due to political pushback, direct threats, and a high-stress, low-reward job environment.
When they’re not coordinating pandemic responses, health departments create education campaigns, monitor disease trends, protect against environmental health hazards, and connect residents with healthcare and other support services. The state and federal government chronically underfund public health, and many health departments, particularly those in rural areas, are ill-equipped to carry out their duties.
In a first-of-its-kind study, Owsley and team looked at the scope of public health practice in urban and rural communities across the country. They asked health departments in 500 communities if they were performing 20 public health activities that federal guidelines identify as critical for improving community health.
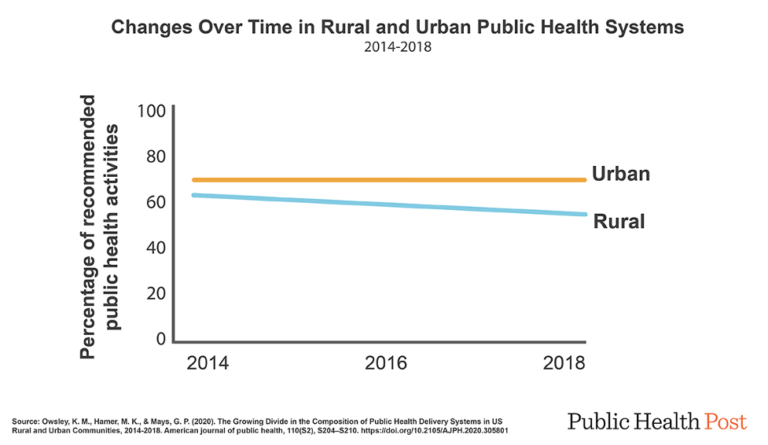
Rural communities engage in fewer recommended public health activities than urban areas. And the activity gap between rural and urban areas health departments is growing. The scope of recommended activities implemented in rural areas declined between 2014 and 2018, whereas activity in urban areas increased.
The federal government has pushed multiple initiatives to strengthen health departments over the past decade, including opening up new funding streams through the Affordable Care Act and providing new opportunities for private partnerships. Rural health departments operate with small budgets and few staff, so they often don’t have the resources to implement new initiatives. Further, many federal initiatives require health systems to compete for funding or limited project spots. Rural departments tend to lose out to better-funded, better-staffed urban departments.
Life expectancy, infant mortality, chronic disease, and cancer outcomes are all worse for rural populations than for their urban and suburban counterparts. And the disparities are growing. By drawing on what works for rural health systems — like neighboring towns or counties pooling resources — local public health systems could play a significant role in reducing rural disparities during the Covid-19 pandemic and beyond.
Databyte via Owsley KM, Hamer MK, Mays GP. The Growing Divide in the Composition of Public Health Delivery Systems in US Rural and Urban Communities, 2014-2018. Am J Public Health. 2020;110(S2):S204-S210. doi:10.2105/AJPH.2020.305801. Visualization by Tasha McAbee.



