Fast, Cheap, Harmful: The Hidden Cost of Ultra-Processed Foods
Reliance on ultra-processed foods can reshape hormones and metabolism, with effects on fertility, pregnancy, and long-term health.

Read Time: 3 minutes
Published:
Ultra-processed foods now stretch from the frozen aisle to the drive-thru, showing up at breakfast, lunch, and in late-night snacks. Instant noodles, sugary breakfast cereals, and—a college favorite—Hot Pockets, offer speed and low cost, but new research links this convenience to serious harm for men’s metabolic and reproductive health.
A recent nutritional intake study led by Jessica M. Preston examined how ultra-processed foods affect health in men aged 20-35. Over the course of three weeks, a group of 43 men rotated between ultra-processed and unprocessed diets. During the ultra-processed weeks, approximately 77% of calories came from industrially prepared foods in the highest NOVA category, including packaged ready meals, refined breads and cereals, processed meats, and sweetened drinks and desserts. During the unprocessed weeks, about two-thirds of calories came from whole or minimally processed foods like vegetables, fruit, whole grains, beans, eggs, and plain yogurt, with almost no ultra-processed products.
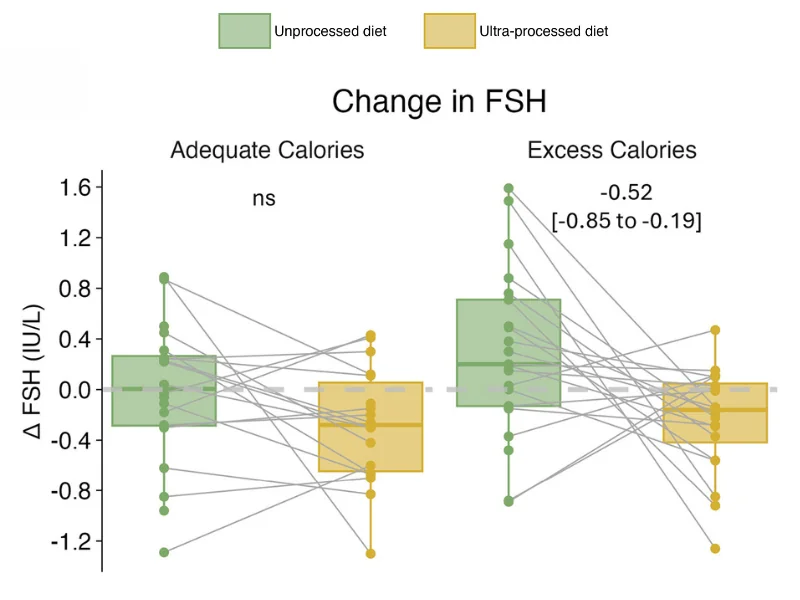
Even when the meals were matched for calories, men gained about one kilogram more fat on the ultra-processed diet, and markers like LDL cholesterol and blood pressure shifted in an unhealthy direction. The figure below zooms in on follicle-stimulating hormone, or FSH, which helps the testes make sperm. Each dot shows a man’s hormone levels before and after each diet.
On the ultra-processed plan (in yellow), most lines tilt downward, meaning FSH levels declined. The drop was strongest in the group given an extra 500 calories a day (on the right), a surplus that drives faster fat gain and puts added strain on the heart and blood vessels. In lab tests, sperm quality also began to slip, with total motility, or how well sperm move, trending downward. Together, higher fat mass, lower FSH, and less active sperm point toward poorer fertility and may signal higher risks for future heart disease.
The study also picked up changes in thyroid and appetite hormones, which help regulate energy use, hunger, and mood. These shifts line up with global concern about sperm counts falling by more than half in the past 50 years and growing rates of metabolic diseases, such as diabetes. Global diet changes, as well as the levels of phthalates, a chemical often used in food packaging, interact to interfere with hormone signaling.
Heavy reliance on ultra-processed foods in young adulthood can quietly reshape hormones and metabolism, with ripple effects on fertility, pregnancy, and long-term heart and brain health. Small shifts toward beans, whole grains, fruits, and vegetables can improve markers like blood pressure and cholesterol, but no one shopper can fix a food system built around ultra-processed options. Policies such as front-of-package warning labels, soda taxes, and stronger school meal standards can help make healthier foods the easier choice.