Disparities in Telehealth Access
Though telehealth use has largely increased since 2020, gaps in use persist among rural and low-income adults, likely driven by a lack of access to and information about these services.
Read Time: 2 minutes
Published:
We associate the use of telehealth services and speaking to our doctors by videoconference with the COVID-19 pandemic. But the trend started several years pre-pandemic in some areas. In 2018, 75% of hospitals in urban areas used telehealth services compared to 58% in rural areas.
Since 2020, however, demand for and access to telehealth services have increased rapidly. Federal funding for telehealth services has increased as a result, and states have relaxed the set of requirements for providers, including allowing clinicians to treat patients outside of their state jurisdiction.
Researcher Jamie Ko and colleagues analyzed data from the nationally representative COVID-19 Unequal Racial Burden (CURB) survey to understand attitudes and barriers impacting telehealth use in rural and low-income communities where telehealth use continued to be used at lower rates during the pandemic.
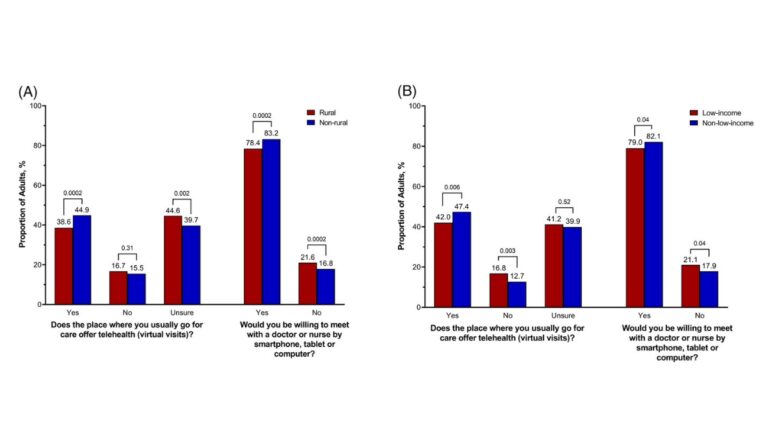
As seen in the figures above, 38.6% of adults in rural communities reported they had access to telehealth services compared to 44.6% in urban areas between December 2020 and February 2021 (graph A). Among low-income adults (graph B), 42% of respondents reported having access compared with 47.4% of other adults. Interestingly, a large proportion of respondents reported being unsure if their provider offered telehealth services at all. The researchers also found that most respondents were willing to use telehealth services.
Ko and colleagues conclude that lack of access and lack of awareness of telehealth services are the main drivers of telehealth disparities in the United States. They recommend educational campaigns and community outreach programs to spread awareness of telehealth services offered at rural and low-income healthcare facilities.
Of note, many respondents reported a language barrier limiting use of telehealth services and Spanish-speaking adults often lacked access to translators for virtual visits. Therefore, the researchers also recommend incorporating automatized interpretation provision into existing telehealth services.
Databyte via Jamie S. Ko, Sherine El-Toukhy, Stephanie M. Quintero, et al. Disparities in telehealth access, not willingness to use services, likely explain rural telehealth disparities. Journal of Rural Health, 2023.