Beyond the Hospital: Remote Care, Lower Costs
Remote monitoring devices offer a promising way to track patient vitals and alert providers to changes before they become life-threatening.

Read Time: 2 minutes
Published:
Hospitalized patients are monitored 24/7. Vital signs like heart rate, oxygen levels, and blood pressure help doctors catch serious problems early. But once discharged from the hospital, patients are on their own. At home, patients may miss early signs of complications and end up back in the emergency department or being readmitted to the hospital within days.
Hospital readmissions disrupt patients’ lives and strain the overcrowded health system. In the U.S., the average cost of a readmission is $15,200, adding up to $52.4 billion annually. But remote monitoring devices that patients can use at home offer a promising way to track vital signs and alert providers to changes before they become life-threatening.
To understand how remote monitoring technology can reduce hospitalizations, Sara Margosian and colleagues analyzed data from more than 1,700 patients in the Patient Monitoring at Home program. This program provided patients with a thermometer, blood pressure cuff, pulse oximeter (to measure blood oxygen levels), digital scale, and a tablet to report and transmit their daily measurements and symptoms. A medical team reviewed this information and referred patients to higher levels of care when needed.
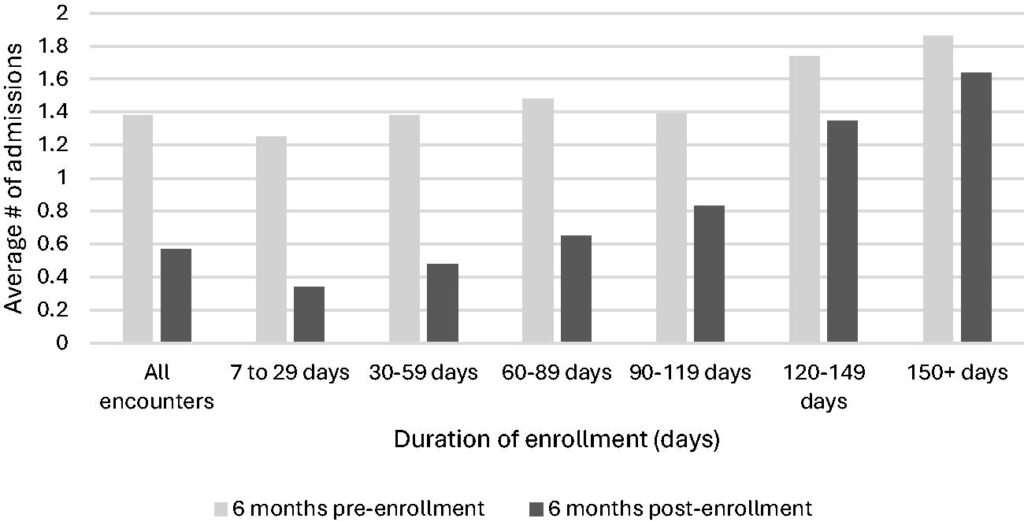
The researchers then compared the average number of hospital admissions in the six months before and after patients enrolled in the remote monitoring program. Hospitalizations dropped by 59% during the 1-2 month remote monitoring period. These benefits persisted, and six months after enrollment, hospital readmissions remained 49% lower than before the program began.
This program has more than paid for itself, with a $12 million return on investment due to avoided hospitalizations. Such programs are particularly helpful for people who face barriers to in-person care: the elderly, immunocompromised, and those living in rural areas or managing chronic illnesses. These groups also face a disproportionately high risk of hospital readmission, making remote monitoring a key tool for targeting health disparities.
Remote monitoring is not yet a standard benefit across health insurance plans. The Patient Monitoring at Home program was successful, in part, because Medicare and other insurers temporarily relaxed telehealth billing regulations in response to COVID-19. Congress recently extended these rules through September 2025, but after that, the future of telehealth is unclear.
What is clear is that telehealth works, and its value extends beyond emergencies. Backed by evidence of clinical benefit and cost savings, the study authors call on policymakers and health leaders to expand telehealth and make remote monitoring a standard of care, not just an emergency fix.