BCRA Undercuts Opioid Treatment
The Better Care Reconciliation Act (BCRA) creates a $45 billion fund for opioid use disorder (OUD) treatment. However, this amount is unlikely to overcome Medicaid spending restrictions proposed in the bill.
Read Time: 2 minutes
Published:
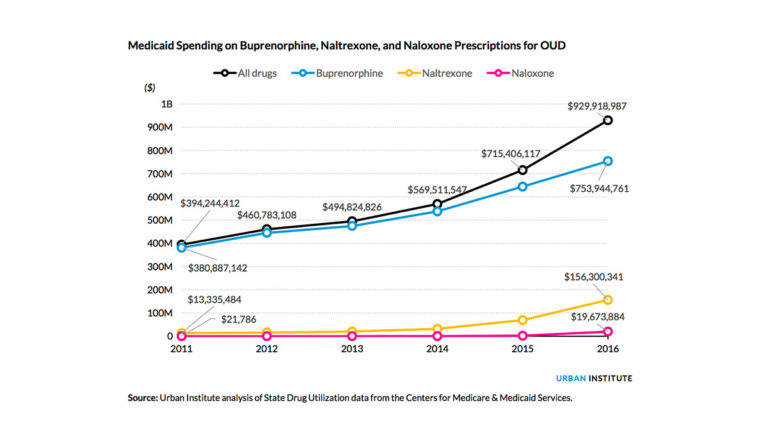
The revised Better Care Reconciliation Act (BCRA) creates a $45 billion fund opioid use disorder (OUD) treatment. The revised bill is a little more generous than its previous iteration that offered $2 billion. This amount, however, will likely not be enough to overcome the Medicaid spending restrictions proposed in the bill that will dramatically cut OUD spending. According to research from Lisa Clemans-Cope and colleagues at the Urban Institute, Medicaid spending on OUD treatment increased by 136% from $394 million to $930 million between 2011 and 2016. It is important to note that the data used did not include methadone, one of the most effective treatments for opioids, meaning the costs are an underestimation.
Before the Affordable Care Act (ACA), access to OUD treatments for low-income adults was difficult due to either lack of health insurance or the cost of the prescription. Thousands of low-income adults gained coverage under Medicaid because of the ACA and subsequently, access to OUD treatments. Buprenorphine, one of the OUD treatments analyzed above, is covered in all Medicaid programs.
Some states will be affected more than others by the Medicaid cuts due to their rapid growth in OUD treatment spending. States that decided to expand Medicaid and had high overdose mortality rates, such as Massachusetts, Rhode Island, Ohio, Kentucky, and West Virginia, will particularly be hurt by spending constraints. West Virginia, for example, spent $25 million on OUD medication in 2016 which is a 431% increase from 2011.
The 45 billion-dollar question here is whether pledged opioid fund is enough to fill the void that the Medicaid spending cuts create and tackle the opioid epidemic. The Urban Institute study only considers the medication costs of OUD treatment. When factoring in the costs of treating comorbid conditions for OUD such as hepatitis C and HIV/AIDs, the estimates of need far exceed the amount allotted. In fact, Dr. Richard Frank of Harvard Medical School estimates the cost to be $183 billion over 10 years in order to “address this population’s healthcare needs stemming from the lost coverage opportunities caused by the AHCA with an epidemic’s costs growing at a minimum of 5.7 percent per year.”
Databyte via Lisa Clemans-Cope, Marni Epstein, and Genevieve M. Kenney, Rapid Growth in Medicaid Spending on Medications to Treat Opioid Use Disorder and Overdose. Urban Institute.