If BBL Safety Measures Exist, Why Are Mortality Rates So High?
Despite the efficacy of ultrasounds in reducing mortality during Brazilian butt lift procedures, many surgeons are opposed to using them.

Read Time: 2 minutes
Published:
The hourglass figure (a slim waist with full hips and bust) has long been an ideal body type for American women across eras, and remains an ideal to this day. Social media has only amplified this beauty standard, with influencers like Kylie Jenner promoting the physique to millions. As a result, curvier bodies have become more common, whether natural, filtered, or enhanced. Brazilian butt lift (BBL) surgery offers a fast track to achieving this look.
BBLs transfer fat from areas like the belly or back to the hips and butt. Though it’s the third most common body surgery in the U.S., it’s also the deadliest. About 1 death occurs every 3,000 procedures. In comparison, traditional liposuction has a much lower death rate (2.6 to 20.6 deaths per 100,000 procedures). The main cause of BBL-related deaths is fat being accidentally introduced into the bloodstream, a fatal phenomenon known as fat embolism.
In the absence of widespread mandated guidelines, the BBL task force issued an advisory that cites using specific equipment and injecting fat above the muscle, a practice shown to lessen fatal complications.
Recently, ultrasound guidance has also been observed to reduce fatal complications during these procedures. Despite the benefits, ultrasound guidance is only required in Florida. This raises a critical question: Why isn’t ultrasound required across all states?
Emily R. Finkelstein and associates surveyed board-certified plastic surgeons to assess their opinion and knowledge on BBL risks, mortality, and safety practices. An online survey was sent to 1,791 surgeons. Of the 178 respondents, 77% performed BBL procedures.
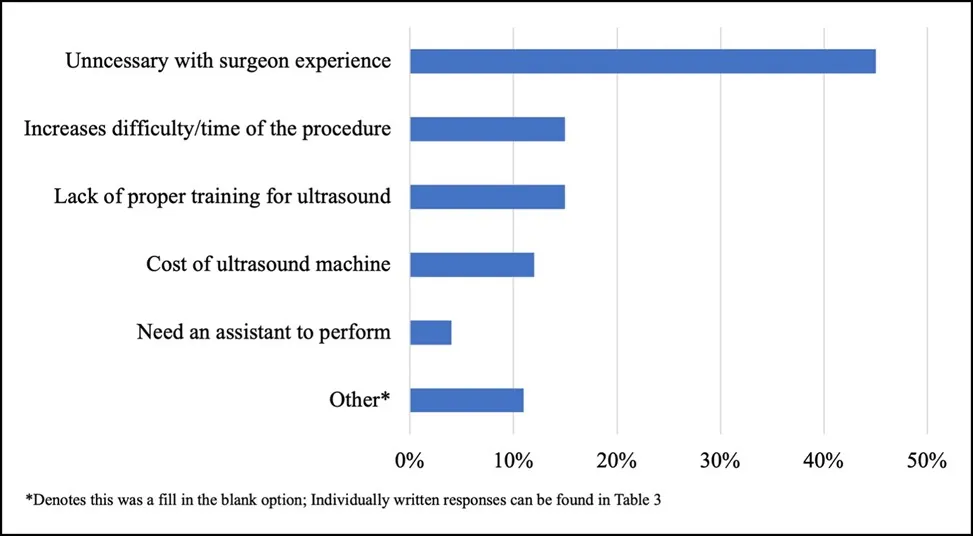
A large portion of respondents (60%) opposed mandatory ultrasound regulations. Many believed ultrasound to be unnecessary for BBL procedures, especially if the surgeon is experienced.
While 94% of respondents correctly identified fat embolism as the main cause of BBL fatalities, 20% accurately estimated the current mortality rate, and more than half of the respondents significantly underestimated BBL-related death rates.
Despite evidence supporting the efficacy of ultrasound-guided BBLs, many surveyed plastic surgeons appear to believe that experience and technique alone are sufficient to reduce mortality. The observed knowledge gaps in this study suggest recent educational efforts have not been enough. Tighter regulations, improved training, and stronger support from the plastic surgery community could help reduce BBL-related deaths and improve patient safety.



