Ron Sims: How Where You Live Affects Your Health
Sims sat down with PHP’s Jonathan Gang to discuss his career, the future of the ACA and the role that public health will play in fighting for people’s access to healthcare over the next four years.

Read Time: 9 minutes
Published:
Ronald Cordell “Ron” Sims is the former Deputy Secretary of the United States Department of Housing and Urban Development (HUD). Since 2014, he has served as the volunteer chair of the Washington Health Benefit Exchange Board, where he is engaged in health, education, environmental, and social equity issues.
Over his long career in public service, Ron Sims has always fought for healthy communities. From 2009 to 2011 Sims was the Deputy Secretary of the Department of Housing and Urban Development. Before that, he served as the County Executive of King Country, Washington for 12 years, working on policies that prioritized affordable housing, climate change, and social justice.
Now happily retired, Sims has served as the volunteer chair of the Washington Health Benefit Exchange Board, the group responsible for implementing the Affordable Care Act in Washington State, since 2014. Sims sat down with PHP’s Jonathan Gang to discuss his career, the future of the ACA and the role that public health will play in fighting for people’s access to healthcare over the next four years.
PHP: You’ve had a long and distinguished career in public service, from King County to the Department of Housing and Urban Development to the Washington Health Exchange. In broad terms, what role has public health played in your career?
Sims: I can’t think of a year when public health did not play a role in my career. When I was first elected as a county council member, public health reported to my committee. Then, when I became executive of King County, public health was going through a significant transformation, a merger of two governments at one time. We were looking at how we would be able to sustain public health and the new roles that we wanted it to play in our rapidly growing region. When I got Housing and Urban Development, I brought a lot of the work that had been done in public health with me. Particularly, a study that I had asked public health to do.
When I was the county executive I had a report from a group called the Joint Center that had identified that 36% percent of African Americans under the age of 30 would have nothing in common with America but their death. So, I brought that back to one of my staff who was a demographer, a young man named Chandler Felt. I had a rule, which is that if I gave you information, I wanted you to think it through. It wasn’t that I would be in a hurry to get it, but I was going to give it time to grow and mature. I call that “Smart people be smart.”
So, several months later, I asked about whether they were close to being finished with their analysis and they asked for two more months, which I gave them. They came back with a report that disturbed them, which was our ability to determine life outcomes such as lifetime earning of children and cause of death by zip code with incredible precision.
When I went to the US Department of Urban Development, I brought that with me. We continued to use that tool and applied it on a national basis by reminding jurisdictions that a zip code is not just an address. It is a life determinant . We needed to refocus our attention on why that happens and try to figure out whether we could make these life determinants positive.
PHP: And what are some of the ways that you’ve worked to address that issue?
Sims: I think there are several. One thing is that we noticed that neighborhoods that have wide sidewalks, community gathering points, many parks, that are well-lighted, and well vegetated, that’s really important. Canopy cover is very important. We always do better in what’s called the grasslands than we do in concrete. And the data screams out loud that we need to do more of that.
Neighborhoods that were considered to be “nice” had all of that. Neighborhoods that were poor lacked an organized system of parks and playgrounds. They had narrower sidewalks. They were not well lighted. They did not have places for people to sit and watch the neighborhood or for people to walk around safely.
We realized that the built environment had significant epigenetic consequences for people. A neighborhood could either soothe them or it could bring a sense of wanting to escape or flee. If you look at cortisol levels, we see that flight response. If you have that flight response when you go to the classroom of a school, you can’t learn because the information you’re getting is being packaged differently than a student that comes in and is very relaxed.
Interestingly enough, if you take a person who is in those neighborhoods and you move them to a neighborhood that’s considered to be a better neighborhood, one that’s well vegetated, has wider sidewalks, has good lighting, that has a capacity for people to relax and feel safe, they do better. Now we know that for people who have moved, their lives change. We realized that the built environment has significant consequence.
PHP: So, what’s the way forward to address this problem?
Well, let me talk about public health and its role.
If you go into public health, your voice has legitimacy. But the issue is not to make it a traditional health issue, like how do you treat diabetes or how do we deal with obesity or immunizations? All of which are really important. It’s about working with the other schools. For instance, if you talk about a community design, you’ve got to talk about planners. You’ve got to talk about people who are in urban agriculture, or landscape architects. Transportation planners. Our assumptions are that those schools are easy to communicate with, and they’re not. So, public health has to be the driver at getting people out of their lanes. Break down the silos so that we can say “all of these other elements are really, really important.” We’re never going to have a discussion unless public health people see themselves as being catalytic and being able to communicate with other disciplines about how we resolve complex issues in those neighborhoods.
There’s a lot of work to be done, but it requires new skills. You’re going to be in a room full of bright, skilled people and you have to understand where they’re coming from and the language that they use. The one thing you do when you come out of any graduate school I know of is you develop an art form: the use of a particular language to describe something. But a landscape architect might have a whole different vocabulary than you in looking at the same problem.
The key is to listen and learn. Public health people have to be, in my opinion, the catalyst. The people who are going to break those walls and invite other people to be a part of the solution. And to listen to them so that we can see “here’s our public health issue that we are looking at, and here are the roles that you can play to ensure that we have a healthier population.”
Public health people have to be, in my opinion, the catalyst. The people who are going to break those walls and invite other people to be a part of the solution.
PHP: We are entering an uncertain time for the country and especially the ACA and public health in general with the results of the last election. So what do you think are some of the biggest challenges that we’re going to face over the next four years in terms of public health?
I think that the changes will not be as dramatic on the public health side as we think, because it’s not the target. What is disturbing is that there are people who believe that people should not have healthcare, which stuns me in a modern age.
I think some of the early rhetoric is now dissipating over how much of the ACA can be rejected. For instance, in my state of Washington, a columnist came out and said here are the percentage of people who have either had Medicaid or lower cost insurance. All of those were counties that President-elect Trump won. The blue counties were not the ones that had the highest percentage of people who were in the ACA either by number or percentage.
I think what’s going to happen is that as this discussion goes on is we’re going to see the areas that President-elect Trump won are the areas that are most dependent on the ACA. And I think that most people want to strengthen their base, they don’t want to weaken it. Taking away health insurance will do that.
PHP: As someone in public service, what is your plan for the next four years? What are you hoping to fight for?
Since those meetings have already started, I think many of us now are trying to figure out what are the next steps for insuring that people will continue to have full health coverage. That’s going to be really, really critical, because that can’t fail. It creates too many problems.
I want to continue to be an advocate for extensive research into things like pandemics, because we’re going to have one. The issue is how quickly we can mobilize, but we’re going to have one. There’s just too many people on the planet, and viruses love hosts. We’re going to get viruses that do what viruses do, which is move very, very quickly from one human being to another.
What we’re not doing well is looking at some underlying causal factors. You know, and a lot of those are based upon diet, mobility issues. We’re still going to have to deal with obesity issues, diabetes issues, heart attack issues. We’re still going to have to look at what is a healthy child. How do we increase the learning capacity of children by making changes to the built environment in particular? What constitutes really good health? That will be our biggest challenge.
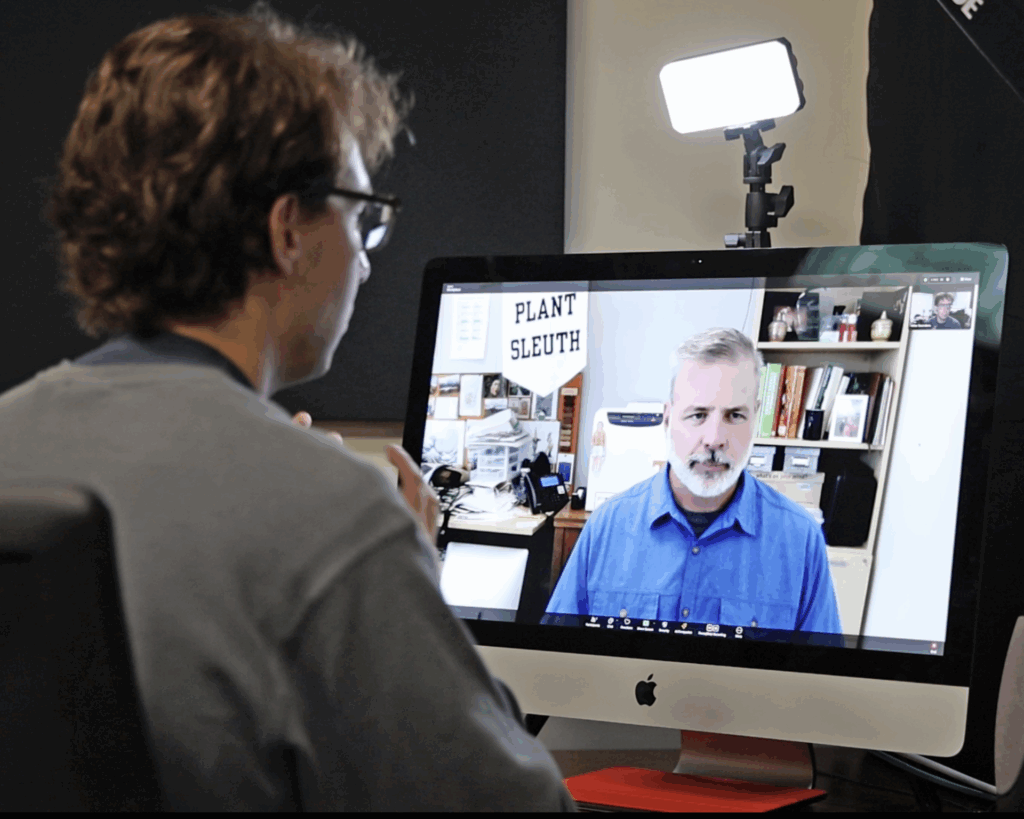
Photo: Ron Sims at Boston University School of Public Health Dean’s Symposia: How Does Where You Live Affect Your Health?, December 1, 2016, courtesy of Boston University School of Public Health Communications Office.