When Lies Go Viral, So Does Disease
The online response to COVID-19 highlighted how social circles often shape people's susceptibility to misinformation.

Read Time: 2 minutes
Published:
As the COVID-19 pandemic unfolded, health misinformation (false or inaccurate health information that contradicts current scientific consensus) about the virus and vaccines spread rapidly online. These misleading claims shaped real-world behavior, fueling vaccine hesitancy and resistance to public health guidance.
Unlike disinformation, which is spread with deliberate intent to deceive, health misinformation can spread unintentionally and still harm public health, discourage vaccination uptake, reduce mask use, and erode trust in public health institutions.
A study led by Matthew DeVerna and colleagues built a simulation model (SMIR) using social media, voting, and mobility data to estimate how misinformation spreads and affects infection risk. In the model, people become misinformed after exposure and then engage in behaviors that increase their likelihood of contracting COVID-19. Here, “infection” refers to predicted viral contraction, not just exposure to misinformation.
In a worst-case scenario, where people are led to believe misinformation after just one exposure to low-credibility content (NewsGuard score <60), peak infection rates are projected to be six times higher than in a best-case scenario with a population more resilient to misinformation. In the worst-case scenario, the infection wave also hits two weeks earlier and is predicted to infect 14% more people (roughly 47 million additional Americans). This translates to more than $143 billion in health care costs.
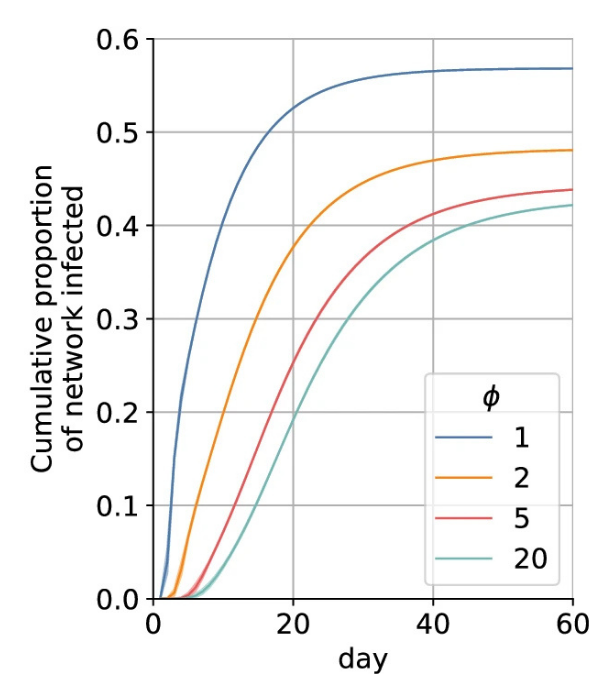
The spread of misinformation depends on how easily people are swayed by their social circles. A lower ‘resilience threshold’ (as indicated by Φ on the graph above) means only a few misinformed friends can convince someone, accelerating both misinformation and disease. The lower the resilience (Φ=1), the greater the proportion of their network infected.
Misinformation harms everyone, not only those who ignore public health guidance. When people skip vaccination, decline testing, or ignore distancing, infections rise, community transmission grows, and even those who follow guidance face a higher risk. This weakens the protection from individual compliance and turns misinformed choices into a population-level threat.
COVID-19 showed how false claims can magnify an outbreak and undercut strong public health measures. Going forward, public health leaders should treat misinformation preparedness like outbreak preparedness by building early detection systems and forming strong community partnerships to protect public trust and collective health.