Surviving the Stroke Belt
Adults living in the Stroke Belt were 1.2 times more likely to suffer a stroke than their counterparts living elsewhere.

Read Time: 2 minutes
Published:
Every 40 seconds, an American suffers from a stroke. As the country’s fifth leading cause of death, a stroke occurs when blood flow to the brain is blocked. Subsequent brain damage causes physical and mental impairment, compromising life expectancy. Smoking, physical inactivity, and high-fat diets can elevate stroke risk. Fixed factors like age, gender, and cardiac history also contribute to the risk. Despite growing death rates, nearly 1 in 3 adults is unaware of symptoms.
Compared to other regions, southeastern U.S. states have such drastically higher mortality rates (20%) that they earned a nickname: the Stroke Belt. This belt includes eight states: Alabama, Arkansas, Georgia, Louisiana, Mississippi, North Carolina, South Carolina, and Tennessee.
An observational study identified geographic differences in stroke prevalence, demographics, risk factors, and quality of life among 18,745 U.S. adults. Using CDC data, the researchers analyzed the effects of modifiable risk factors—those preventable through healthy lifestyle practices—across Stroke Belt and Non-Stroke Belt states.
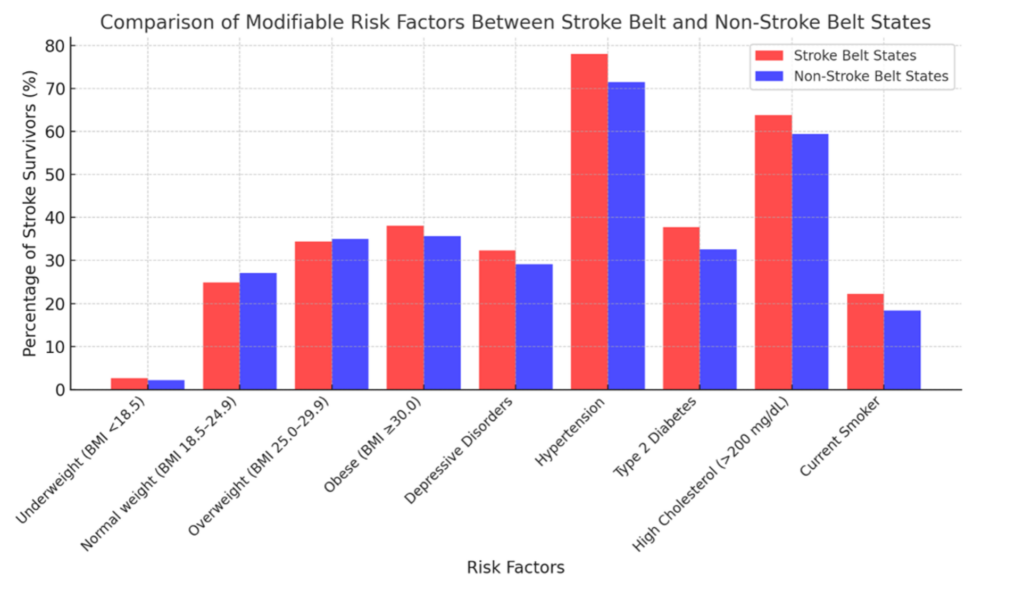
Adults in the Stroke Belt were 1.2 times more likely to suffer a stroke than their counterparts elsewhere. Risk factors were also more common in the Stroke Belt, particularly hypertension (78%) and high cholesterol (63.8%). Even modest differences in risk factor prevalence contributed to higher stroke-related mortality.
The survival gap is especially striking: only 17.7% of survivors lived in the Stroke Belt, compared to 82.3% from other states. Populations with historically limited health care access (i.e., non-Hispanic Blacks, American Indian/Alaska Natives, and those with lower income and education) were at greater risk of stroke. Survivors also reported lower quality of life, facing difficulty with daily tasks like climbing stairs and bathing independently.
In 2024, the American Heart Association updated stroke guidelines to prioritize healthy sleep, diet, and exercise routines, alongside early medical intervention as prevention measures. Targeted education and outreach are essential, specifically in high-risk communities.
Initiatives like Live to the Beat, originally launched among Black adults, can be expanded to low-income and racially diverse groups and teach heart-healthy practices through exercise, healthy eating, and smoking cessation. School-based programs like FAST and JumpRope for Heart are equally important, raising awareness about heart health from an early age. Stroke education is critical—it can mean the difference between a preventable death and a long, healthy life.