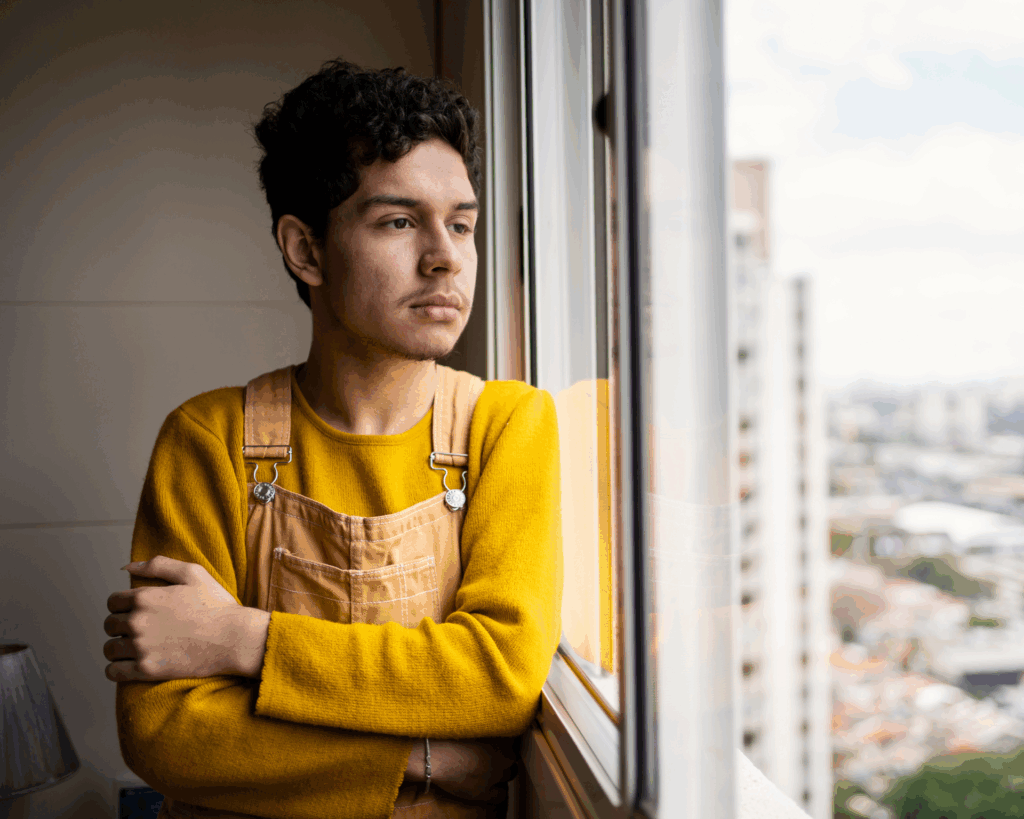
Onyebuchi Arah
Oluwatobi Alliyu profiles Dr. Onyebuchi Arah to highlight current trends of noncommunicable diseases and social inequities in the US and around the world.

Read Time: 4 minutes
Published:
Onyebuchi Arah is a professor in the Department of Epidemiology at the Fielding School of Public Health and an affiliated professor in the Department of Statistics at the University of California, Los Angeles. He currently works on epidemiologic methodology, especially bias analysis and causal inference, clinical epidemiology, computational epidemiology, and global social epidemiology.
Public Health Post: What is the current state of noncommunicable diseases in the US and abroad? How are they the same and how do they differ?
Onyebuchi Arah: Noncommunicable chronic diseases (NCDs) have dominated the west, but this is increasingly becoming the case in lower-income countries or resource-poor settings around the world. Lower-income countries are beginning to experience the arrival of noncommunicable chronic diseases like stroke and cancer, which are starting to represent a higher burden of disease. In other countries, there’s an emergence of a double burden from infectious diseases that are still present, although they’re declining, and noncommunicable diseases that are on the rise. This coexistence of infectious and noncommunicable diseases can be quite harmful and devastating. Diseases tend to affect the vulnerable. That is, those who have less resources by definition or due to societal structure—the poor, people of color, sexual minorities. When we try to reduce the burden of diseases, the gains accrue faster to those at the top of the socioeconomic ladder than those at the bottom. In some cases, we’re actually paradoxically widening the gap while decreasing the burden of disease in absolute terms.
Once you’ve recognized such a trend, how do you address the situation to decrease inequity?
Society has to reflect on how its existing institutional mechanisms work—how are we valuing people’s education? How many resources are we giving to those we have decided to value more than others? How is that disproportionately helping them to the detriment of others? Society has to recognize that its current mechanisms are not working for vulnerable populations. We have to devise ways to prioritize and increase our investment in such populations.
Who are the key decision makers in the position to mobilize investments in the way you’ve described?
The typical suspects are politicians because they set the tone for society and what it wants to be. But civil society (companies, individuals) also has a role to play. We ourselves decide as a group what kind of society we want. We elect politicians and, through civil engagement, we communicate what we want, what we’re going to vote for, and what we support.
Could you give an example of what an investment to decrease existing inequities would look like?
Investing in dducation. In the US, there is a growing divide in educational skills among different populations. There is a gap between those who are highly educated and have the skillsets to thrive in today’s world and those whose education and skillsets are ill-matched for today’s digital environment. They are unable to compete in a society that has gone very global and technological.
The WHO’s Global Action plan for NCDs aims to reduce deaths from NCDs by 25% by 2025. Do you think the US is on track? What factors are leading to or preventing progress?
Yes and no. Yes, because we’ve seen some positive changes in areas like cardiovascular disease and cancer. No because new things like substance abuse and mental health issues, which we are not close to being ready for, are surfacing. We are not investing enough in people who stand to gain the most from health interventions. Our investments tend to favor society’s elite. While this group benefits from health interventions, the biggest absolute gains lie in addressing the needs of vulnerable populations.
Is there a need for an overhaul of the US health care system in order for us to reach the people who need it most?
First, we have to decide that we want to provide access. We have to start looking for cost effective ways to provide access to health care. We are currently not doing this because we haven’t convinced ourselves that it is necessary. The price we’re paying for healthcare is just astronomical and mindboggling.
Social epidemiology deals with the way social structures, institutions, and relationships influence health. What are some key insights that have stemmed from analyzing NCDs from a social epidemiological perspective?
We’ve learnt that the decline of NCDs, in absolute terms, are socially patterned. In other words, those who bear the highest burden of disease are socially definable. They are people society has defined as being different—sexual minorities, people of color, people who are poor, inner-city dwellers. They do not enjoy the same success rates as other groups because we do not invest enough in their determinants of health—things like quality housing, employment, and non-discriminatory laws. Social factors determine who gets what, who is helped, who pays, and who is forgotten. These are the lessons we’ve learnt from analyzing NCDs from a social epidemiological lens.
Photo courtesy of Onyebuchi Arah