Correction-ing Community Health Policy
Researchers modeled and simulated the transmission of COVID-19 between a U.S. correctional facility and its local community to analyze the benefits of testing and quarantining incarcerated people and the risks of spillover infections.
Read Time: 2 minutes
Published:
COVID-19 incidence is 5.5 times higher in U.S. state and federal prisons than in the broader community. The super spreading potential of correctional facilities received public attention early in the pandemic due to rapid spread within these places and links to infection within local communities.
We modeled and simulated the transmission of COVID-19 between a U.S. correctional facility and its local community to analyze the benefits of testing and quarantining incarcerated people and the risks of spillover infections. Spillover infections occur when formerly incarcerated people return to the community while infectious or because people who live in the community work in the facility and acquire infection. Our results indicated that a single infected incarcerated person in a jail is more likely to cause a spillover infection in the community than cause a major outbreak within the same facility.
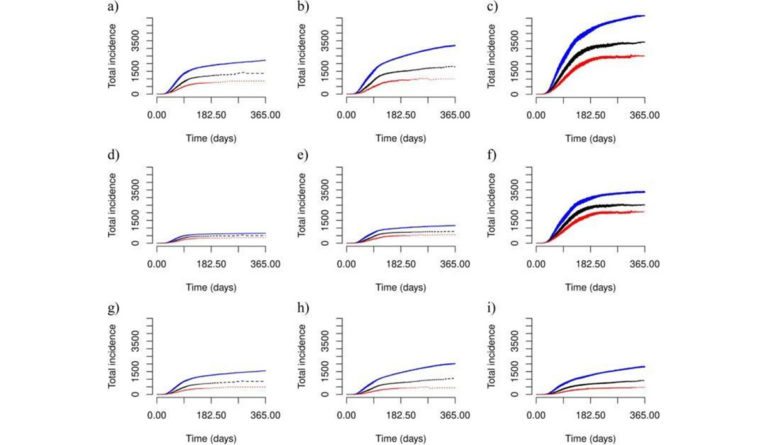
The series of figures shows the effect of varying testing and quarantining practices on COVID transmission over one year. Our analysis is based on a hypothetical jail that confines 820 people and employs 420 community members. The figures in the left column show findings from a correctional facility based in a small community, the middle column a medium-sized community, and the right column a large community. We predict total incidence when incarcerated people are not tested or quarantined (blue curves), when testing and quarantining in the jail occurs less frequently than in the community (black curves), or at the same rate as the community (red curves).
We found that testing and quarantining incarcerated people reduces the incidence of COVID-19 overall (figures a – c), within the community (figures d-f), and within a jail (figures g-i). Our results show disparities in the use of testing and quarantining between the community and facility can negate their potential benefit.
The health of incarcerated people affects the risk and magnitude of COVID-19 outbreaks in local communities. Yet, correctional facilities and local communities often operate autonomously. Effective community health policy must consider the wellbeing of all people in communities, including those detained in their local correctional facilities.
Databyte via Scott Greenhalgh, Ashley Provencher, Inclusive health: modeling COVID-19 in correctional facilities and communities. BMC Public Health, 2022.