Causes and Costs of Global COVID-19 Vaccine Inequity
The persistent inequity in COVID-19 vaccination rates has had daunting health, social, and economic consequences worldwide.

Read Time: 4 minutes
Published:
The COVID-19 pandemic triggered staggering health, social, and economic costs. More than 7 million COVID-19 deaths have been confirmed worldwide, and estimates of excess mortality are two to three times larger. The pandemic was also responsible for the largest global economic crisis in a century, driving business and school closures to control the spread of infections, disrupting global supply chains and routine immunization, compromising mental health, and increasing learning gaps between poor and rich children.
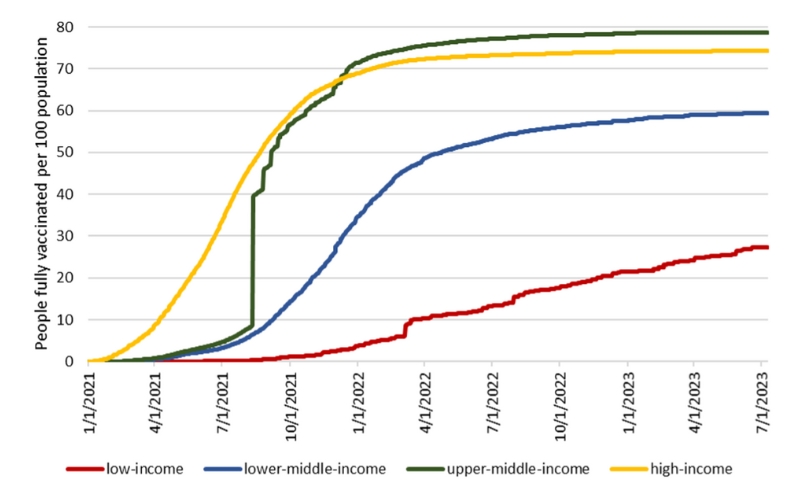
The rapid development of effective and safe COVID-19 vaccines played a key role in containing the costs of the pandemic. Vaccination allowed countries to control the spread of infections, hospitalizations, and deaths; ease travel and other mobility restrictions; and reopen businesses and schools. However, COVID-19 vaccination rollout proceeded unevenly around the world, with higher-income countries starting the vaccination process earlier than lower-income countries.
Overall, 65% of the global population completed the initial COVID-19 vaccination protocol (i.e., two doses for most vaccines). However, the percentage of people who have completed the initial protocol differs starkly across countries, as shown in the graph below: more than 70% of people in high- and upper-middle-income countries compared to only 27% of people in low-income countries. In lower-middle-income countries, 59% completed the initial vaccination protocol.
I recently investigated the factors behind global COVID-19 vaccination inequity and the health, social, and economic costs it triggered. The analysis provides lessons for the management of future pandemics.
Given the high health, social, and economic costs of vaccine inequity, ensuring a more equitable global distribution of vaccines is a key component of pandemic preparedness.
The main contributors to vaccine inequity included vaccine nationalism (i.e., the stockpiling of vaccines by higher-income countries), infrastructure and logistical barriers (e.g., preserving ultra-cold chains and administering vaccines in remote areas), vaccine hesitancy spread by misinformation and mistrust in institutions, and unfair global distribution of vaccine manufacturing capacity. Aside from a few middle-income countries (e.g., China, Cuba, India), manufacturing capacity was limited to wealthy countries, forcing the rest of the world to rely on international vaccine supplies. Manufacturers’ reluctance to share the know-how undermined efforts to expand capacity and global access.
The persistent global inequity in vaccination rates has had daunting health, social, and economic consequences. Those costs negatively impacted all countries, including those that experienced high vaccination rates. A more equal global distribution of vaccines could have prevented many deaths in lower-income countries, and reduced disruptions to childhood immunizations and endemic disease management. Low vaccination rates have been responsible for a slower economic recovery in low- and lower-middle-income countries, which also reported the longest average duration of school closures. These delays widened the already broad educational gap between rich and poor countries. Moreover, a more equitable distribution of vaccines is in the self-interest of higher-income countries as it might have prevented the emergence of new variants and continuous disruptions to global supply chains.
Recent estimates suggest that another event with the mortality level of COVID-19 could occur in 30 to 50 years (i.e., with an annual probability of 2 to 3%). This calls for enhanced investment in pandemic preparedness and prevention—including strengthening surveillance and health care systems, building manufacturing capacity, and accelerating the development of vaccines against pathogens with pandemic potential.
Given the high health, social, and economic costs of vaccine inequity, ensuring a more equitable global distribution of vaccines is a key component of pandemic preparedness. Among other factors, developing local manufacturing capacity through technology transfer agreements and waving of property rights can enhance timely access to supplies in case of emergencies. Failure to overcome existing barriers to global vaccine equity can be tragically shortsighted.